Inhibitory effect of acetamide-45 on airway inflammation and phosphodiesterase 4 in allergic rats1
Introduction
Asthma is a chronic inflammatory disease of the airways, of which lung inflammation and bronchial hyperactivity (BHR) are two distinct characteristics[1,2]. Eosinophils are consi-dered to be the principal inflammatory leukocytes involved in the asthmatic reaction, due in part to the toxic granular proteins they secrete and the membrane products that induce airway epithelial pathology and mucus hypersecretion[3,4]. 3',5'-Cyclic-nucleotide (cAMP) has important regulatory roles in the process of inflammation. Phosphodiesterase 4 (PDE4), which catalyzes the hydrolysis of cAMP to the corresponding nucleotide, 5'-monophosphate, appears to be an attractive target for anti-inflammatory drugs[5,6]. Inhibition of PDE4 results in increased levels of cAMP, which leads to functional inhibition of inflammatory cells such as eosinophils and lymphocytes, and reduced release of inflammatory cytokines such as interleukin-4 (IL-4)[7,8]. There has been significant interest in PDE4 inhibitors as potential therapeutic agents for asthma.
Because asthma has been the focus of much study effort, treatment of the disease has been improved by the implementation of management guidelines in recent years[9]. Such treatments as corticosteroids, β2-agonists, theophylline and leukotriene antagonists have been used as anti-inflammatory agents to control asthma[10]. However, the possible dose-related adverse systemic effects produced by long-term treatment with these drugs are not acceptable in clinical practice[11,12]. Therefore, new anti-asthma agents are required.
A series of new N-(pyridin-4-yl)-(indol-3-yl) alkylamides (44-84) have been prepared in the search for novel antiallergic drugs. Initial studies showed that acetamide-45 inhibited IL-4 and IL-5 biosynthesis and histamine release[13]. We have also previously reported that acetamide-45 has an inhibitory effect on histamine- and methacholine-induced contractions of isolated guinea pig trachea, and that it can inhibit PDE4 activity[14,15]. It was concluded that acetamide-45 was a new antiallergic agent. However, little is known about its effects on eosinophil infiltration in airway and lung function in asthmatic rats. There have been no reports regarding the effect of acetamide-45 on PDE4 activity in the lungs in any animal model of asthma.
Therefore, in the present study, we examined the inhibitory effect of acetamide-45 on airway inflammation and lung function in a rat model of asthma, and indicated a possible mechanism by which the effect might be exerted.
Materials and methods
Animals Male Sprague-Dawley rats weighing 140–160 g were obtained from the Laboratory Animal Center of the Medical School of Zhejiang University (Certificate N
Chemicals Aminophylline, cAMP, and ovalbumin were purchased from Sigma (St Louis, MO, USA). Acetamide-45 was kindly provided by the Department of Organic Chemistry and Medical Chemistry, Faculty of Pharmacy (Nantes University, France). The rat IL-4-specific enzyme-linked immunosorbent assay (ELISA) kit was purchased from Jingmei BioTech Co (Shenzhen, China).
Sensitization and challenge procedure Rats were sensitized by a single intramuscular injection of 10 mg ovalbumin (OVA) mixed with 100 mg aluminum hydroxide in 1 mL of saline. After 2 weeks, these animals were then challenged by exposure for 20 min to aerosolize 1% OVA in saline generated by a jet nebulizer once a day for 7 d. The drugs were administered by intraperitoneal injection before challenge. The doses of acetamide-45 were 5, 10, or 30 mg/kg, respectively, and the dose of aminophylline was 10 mg/kg per day for 7 d. At d 21, the animals were killed, and the lung tissues were immediately removed, frozen in liquid nitrogen, and then stored at -80 °C until analysis.
Measurement of lung function At 24 h after the last antigen challenge, rats were anesthetized with urethane (1 g/kg, ip). The trachea was cannulated and placed in a whole body plethysmograph for the measurement of lung resistance (RL) and dynamic lung compliance (Cdyn)[16,17].
Cell counts in bronchoalveolar lavage Bronchoalveolar lavage (BAL) was performed by flushing the airways with 10 mL/kg saline containing 1% bovine serum albumin and 1000 kU/L heparin sodium through a tracheal cannula. The BAL fluid was pooled and immediately centrifuged at 500×g at 4 °C for 10 min. The supernatant was removed and the cells were resuspended in 1 mL saline containing 10% bovine serum albumin. Counts of the total number of leukocytes recovered in the BAL fluid were carried out using a Neubauer chamber, and differential cell analysis was carried out under a light microscope after Wright-Giemsa staining.
Determination of IL-4 in lung tissue At a ratio of 1 g to 10 mL, homogenized lung tissue was added to 50 mmol/L potassium phosphate buffer (pH 6.0) containing 0.05% NaN3 and 0.1% 3-[(3-cholamidopropyl) dimethylammonio]-1-propanesulfonate (CHARPS). The homogenates were centrifuged twice at 19 851×g, each for 30 min[17]. IL-4 in the supernatants was quantified using a rat IL-4-specific ELISA kit.
PDE4 activity assay Frozen 25-mg pieces of lung tissue were homogenized and PDE4 activity was determined by high performance liquid chromatography (HPLC) as described elsewhere[15,18].
Statistical analysis Data are expressed as mean±SD. Statistical analysis was performed using one-way analysis of variance.
Results
Effects of acetamide-45 on inflammatory cells in the airways of allergic rats In our rat model of allergic asthma, ovalbumin sensitization and challenge caused an obvious increase in inflammatory cells in BAL. As shown in Figure 1, the total number of leukocytes and eosinophils in the OVA group was significantly greater than that in the normal group (P<0.05), but the number of inflammatory cells was depressed when aminophylline (Ami) was administered (P<0.05 vs OVA). Seven days of treatment with acetamide-45 (Ace) at 5, 10, or 30 mg/kg significantly decreased the number of inflammatory cells in BAL caused by sensitization and challenge (P<0.05 vs OVA; Figure 1). There was no statistical difference between the Ace group and the Ami group (P>0.05; Figure 1).

Effects of acetamide-45 on RL and Cdyn in allergic rats After rats were given 7 aerosolized OVA challenges, a significant decrease in Cdyn was induced. However, through sensitization and challenge, RL increased to a level that was significantly greater than that in the normal group. The administration of aminophylline decreased the RL and increased the Cdyn of sensitized and challenged animals. At a dose of 5, 10, or 30 mg/kg, acetamide-45 improved both Cdyn and RL (Figure 2).

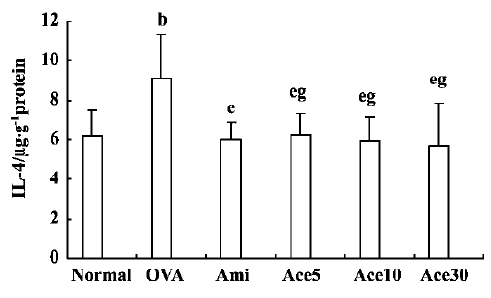
Effect of acetamide-45 on IL-4 in lung tissue in allergic rats As shown in Figure 3, IL-4 levels in the lungs of rats from the various groups were measured. Sensitization and challenge increased the concentration of IL-4 to a level significantly different from that of the normal group (P<0.05). Seven days of treatment with acetamide-45 at concentrations of 5, 10, or 30 mg/kg, or with aminophylline at a concentration of 10 mg/kg, obviously reduced the increase in the concentration of IL-4 (P<0.05).
Effect of acetamide-45 on PDE4 activity in lung tissue in allergic rats Sensitization and challenge increased the PDE4 activity of lung tissue to 503±125 nmol·g-1·min-1, which was greater than that of the normal group (P<0.05). Acetamide-45 at concentrations of 5, 10, or 30 mg/kg inhibited the hydrolysis of cAMP by the PDE4 extracted from lung tissue. The PDE4 activities of the lung tissue were 281±55, 273±57, and 238±36 nmol·g-1·min-1, respectively (for acetamide-45 at concentrations of 5, 10, or 30 mg/kg). As a non-selective inhibitor of PDE4, aminophylline suppressed PDE4 activity to 341±44 nmol·g-1·min-1 at a dose of 10 mg/kg, which was weaker than the activity produced by treatment with acetamide-45 at concentrations of 10 and 30 mg/kg (P<0.05, Figure 4).

Discussion
Acetamide-45, N-(pyridin-4-yl)-[1-(4-fluorophenyl) indol-3-yl] acetamide, is a new anti-inflammatory drug that inhibits the release of cytokines and the activation of eosinophils[12]. It has also been reported that acetamide-45 inhibits the contraction of isolated guinea pig trachea induced by histamine and methacholine[14]. However, the mechanism by which acetamide-45 acts remains unknown. The present study shows that acetamide-45 can suppress the accumulation of inflammatory cells in airways and improve the lung function of allergic rats. We also found that acetamide-45 could inhibit PDE4 activity and reduce the IL-4 level in the lung tissue of allergic rats. To our knowledge, this study represents the first investigation of the effect of acetamide-45 on lung function and PDE4 concentration in the lung in an animal model of asthma.
Asthma is a syndrome characterized by eosinophil infiltration and airway hyperresponsiveness, which occurs via a mechanism that is very complex. It is well known that eosinophils play a critical role in airway damage and dysfunction in asthma. We found that acetamide-45 had an inhibitory effect on eosinophil infiltration in the airways of allergic rats. Not only eosinophils but also other inflammatory cells were decreased in concentration, so that inflammation of the airway in allergic rats was inhibited by acetamide-45.
Inflammation of the airway leads to spasms of the bronchial smooth muscles, mucus hypersecretion, and airflow limitations, which result in pulmonary dysfunction in asthma. The data obtained by a whole body plethysmograph in this study indicate that acetamide-45 improves the lung function of allergic rats produced by sensitization and challenge. Its effectiveness has been demonstrated in two ways. First, the Cdyn of allergic rats increased obviously relative to normal rats at a dose of 5 mg/kg acetamide-45. Second, the RL of allergic rats was reduced significantly by acetamide-45 in the same way. The improvement in lung function produced by acetamide-45 is similar to that produced by aminophylline.
The experiments presented here show that both acetamide-45 and aminophylline repress IL-4 production in allergic rats, but that there is no difference between the two agents. IL-4 is a key cytokine in the development of allergic inflammation. It is associated with the secretion of IgE by B lymphocytes and the expression of eotaxin and other inflammatory cytokines that contribute to inflammation and lung remodeling in asthma[18,19]. A previous study shows that acetamide-45 inhibits IL-4 biosynthesis and release, which is identical to our result[12]. This indicates that acetamide-45 can reduce the release of IL-4 and reduce its concentration in the lung, which results in the inhibition of airway inflammation.
Our study of PDE4 activity shows that acetamide-45 has an inhibitory effect on cAMP hydrolysis of PDE4 in the lung tissue of allergic rats. In a previous study, we demonstrated that acetamide-45 could inhibit the hydrolysis of cAMP by PDE4 extracted from transfected yeast, and that its inhibitory effect was stronger than that of theophylline[15]. The present study also shows that at the same dose (10 mg/kg), the inhibitory effect of acetamide-45 is greater than that of aminophylline, which is a non-selective PDE inhibitor. PDE4 is specific for cAMP, and is predominantly expressed in inflammatory cells. It plays an important role in the regulation of cellular functions in inflammatory and immune cells, and inhibition of PDE4 may be one of the anti-inflammatory mechanisms of acetamide-45.
In conclusion, we have shown that acetamide-45 could improve the lung function of allergic rats produced by sensitization and challenge, and that production of eosinophils in those animals could also be repressed. Acetamide-45 had an inhibitory effect on PDE4 activity in the lung tissue of allergic rats, and the inhibition was stronger than that produced by aminophylline. The present research may provide an experimental basis for further study of this agent.
References
- O’Byrne P. Asthma pathogenesis and allergen-induced late responses. J Allergy Clin Immunol 1998;102:S85.
- Agrawal DK, Bharadwaj A. Allergic airway inflammation. Curr Allergy Asthma Rep 2005;5:142-8.
- Kumar RK, Herbert C, Thomas PS, Wollin L, Beume R, Yang M, et al. Inhibition of inflammation and remodeling by roflumilast and dexamethasone in murine chronic asthma. J Pharmacol Exp Ther 2003;307:349-55.
- Tomkinson A, Cieslewicz G, Duez C, Larson KA, Lee JJ, Gelfand EW. Temporal association between airway hyperresponsiveness and airway eosinophilia in ovalbumin-sensitized mice. Am J Respir Crit Care Med 2001;163:721-30.
- Conti M, Richter W, Mehats C, Livera G, Park JY, Jin C. Cyclic AMP-specific PDE4 phosphodiesterases as critical components of cyclic AMP signaling. J Biol Chem 2003;278:5493-6.
- Wang T, Wang P. Novel approaches to using PDE4 inhibitors for antihypertensive therapy. Curr Opin Investig Drugs 2005;6:283-8.
- Landells LJ, Spina D, Souness JE, O’Connor BJ, Page CP. A biochemical and functional assessment of monocyte phosphodiesterase activity in healthy and asthmatic subjects. Pulm Pharmacol Ther 2000;13:231-9.
- Torphy TJ. Phosphodiesterase isozymes, molecular targets for novel antiasthma agents. Am J Respir Crit Care Med 1998;157:351-70.
- Bousquet J. Global initiative for asthma (GINA) and its objectives. Clin Exp Allergy 2000;30 Suppl 1:2-5.
- Mark A. Phosphodiesterase 4 inhibitors and the treatment of asthma. Drugs 2000;59:193-212.
- Giembycz MA. Development status of second generation PDE4 inhibitors for asthma and COPD: the story so far. Monaldi Arch Chest Dis 2002;57:48-64.
- Norman P. PDE4 inhibitors 2001: Patent and literature activity 2002–September 2001. Expert Opin Ther Patents 2002; 12: 93–111.
- Menciu C, Duflos M, Fouchard F, Le Baut G, Emig P, Achterrath U, et al. New N-(pyridin-4-yl)-(indol-3-yl) acetamides and propanamides as antiallergic agents. J Med Chem 1999;42:638-48.
- Lu YB, Chen Z, Wu M. Acetamide-45 inhibits histamine- and methacholine-induced contraction of isolated guinea pig trachea. Acta Pharmacol Sin 2002;23:152-6.
- Wang K, Chen JQ, Chen Z, Chen JC. Inhibition of human phosphodiesterase 4A expressed in yeast cell GL62 by theophylline, rolipram, and acetamide-45. Acta Pharmacol Sin 2002;23:1013-7.
- Xie QM, Zeng LH, Zheng YX, Lu YB, Yang QH. Bronchodilating effects of bambuterol on bronchoconstriction in guinea pigs. Acta Pharmacol Sin 1999;20:651-4.
- Xie QM, Chen JQ, Shen WH, Yang QH, Bian RL. Comparison of bronchodilating and antiinflammatory activities of oral formoterol and its (R,R)-enantiomers. Acta Pharmacol Sin 2003;24:277-82.
- Tang HF, Song YH, Chen JC, Chen JQ, Wang P. Upregulation of phosphodiesterase-4 in the lung of allergic rats. Am J Respir Crit Care Med 2005;171:823-8.
- Ryan JJ. Interleukin-4 and its receptor: essential mediators of the allergic response. J Allergy Clin Immunol 1997;99:1-5.
- Wills-Karp M, Gavett SH, Schofield B, Finkelman F. Role of interleukin-4 in the development of allergic airway inflammation and airway hyperresponsiveness. Adv Exp Med Biol 1996;409:343-7.
