Influence of dosage forms on pharmacokinetics of daidzein and its main metabolite daidzein-7-O-glucuronide in rats1
Introduction
Daidzein [7-hydroxy-3-(4-hydroxyphenyl)-4H-1-benzopyran-4-one, CAS 486-66-8, Figure 1] is one of the naturally occurring isoflavones present mainly in leguminous plants, especially in soybeans, soy foods and Pueraria lobata Ohwi (Leguminosae). Several epidemiological studi-es in humans have suggested that daidzein intake is inversely associated with the incidence of hormone-dependent diseases, especially breast and prostate cancer[1]. In addition to its putative anticarcinogenic effects, daidzein has also been investigated as an antihyperlipidemic agent and a therapeutic substance to combat osteoporosis[2,3].
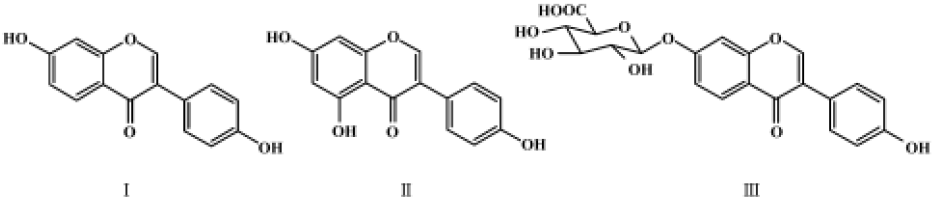
After oral administration, daidzein is subject to glucuronidation at the 7-hydroxyl position, and daidzein-7-O-glucuronide is its main metabolite in human[4] and rat[5] plasma and urine. The pharmacokinetics of daidzein in humans has been the subject of several studies[6-10], but there have been no reports about the pharmacokinetics of its main metabolite daidzein-7-O-glucuronide. Due to its poor hydrophilicity and lipophilicity, the pharmacokinetics of daidzein may be influenced by the dosage form. However, the influence of dosage forms on the pharmacokinetics of daidzein and its main metabolite daidzein-7-O-glucuronide have not been investigated previously. Furthermore, the extent of the influence of dosage forms remains unknown.
In the present study, the influence of two typical dosage forms (solution and suspension) on the pharmacokinetics of daidzein and its main metabolite daidzein-7-O-glucuronide was investigated after oral administration of 20 mg/kg purified daidzein to rats.
Materials and methods
Chemicals and reagents Daidzein and genistein (internal standard) were purchased from Huike Botanical (Xi'an, Shaanxi, China). The purities of these 2 compounds were 99.3% and 98.9%, respectively, which was verified using high-performance liquid chromatography (HPLC) methods. β-Glucuronidase (EC 3.2.2.21, 542 200 units/g of solid) was purchased from Sigma (St Louis, MO, USA). CMC-Na was purchased from Shenyang Chemical Factory (Shenyang, Liaoning, China). Acetonitrile and methanol (Yuwang Chemical Factory, Shandong, China) were of HPLC grade. Other chemicals were of analytical grade. Distilled water, prepared from demineralized water, was used throughout the study.
Preparations of dosage forms A transparent solution of daidzein was prepared by dissolving an appropriate amount of daidzein in 0.9% NaCl solution (water was used as solvent) and adjusting the pH to 7.0 by the addition of 1 mol/L NaOH. A daidzein suspension with good physical stability was achieved by dispersing grinded daidzein in 0.5% CMC-Na solution (water was used as solvent and CMC-Na was used as co-suspension reagent). The concentrations of daidzein in both dosage forms were determined to be 2.0 g/L by a validated HPLC-UV method. The 2 dosage forms were prepared freshly for animal administration.
Instrumentation A Finnigan TSQ API II tandem mass spectrometer equipped with an atmospheric pressure chemical ionization (APCI) source (San Jose, CA, USA), an Agilent 1100 autosampler (Agilent, Wilminton, DE, USA) and a Shimadzu LC-10AD pump (Kyoto, Japan) were used for LC-MS-MS analyses. Analytical data were acquired using Xcalibur 1.1 software (Finnigan) and quantitative processing was carried out using LCQuan software (Finnigan).
LC-MS-MS conditions The LC-MS-MS method used for the determination of daidzein and daidzein-7-O-glucuronide was a slightly modified version of one described previously[11]. The LC separation was carried out using a Diamonsil C18 column (200 mm?4.6 mm ID, 5 mm; Dikma, Beijing, China) and a SecurityGuard C18 guard column (4 mm?3.0 mm ID; Phenomenex, Torrance, CA, USA). The isocratic mobile phase consisted of acetonitrile-water-formic acid (80:20:1, v:v:v) at a flow rate of 0.75 mL/min. The column temperature was maintained at 20 ºC.
The mass spectrometer was operated in positive APCI mode with the corona discharge current set at 4.00 µA. Nitrogen was used as the sheath gas (0.6 MPa) and auxiliary gas (3 L/min) for nebulization. The heated capillary and vaporizer temperatures were set to 280 ºC and 450 ºC, respec-tively. For collision-induced dissociation (CID), argon was used as the collision gas at a pressure of 0.19 Pa. Quantification was carried out using selected reaction monitoring (SRM) of the transitions m/z 255?199 for daidzein and m/z 271?153 for genistein, with a scan time of 0.3 s/transition. The optimized collision energies of 30 eV and 35 eV were chosen for daidzein and genistein, respectively.
Sample preparation To determine free (unconjugated) daidzein, 50 mg/L internal standard solution (genistein, 50 mg/L in methanol) and 50 mg/L water were added to 50 mg/L of each rat plasma sample. NH4H2PO4 buffer (pH 5.0; 200 mg/L of 0.05 mol/L) was added. The mixture was vortexed for 10 s and extracted with 2 mL n-hexane-diethyl ether (1: 4, v/v) by shaking for 10 min. After centrifugation at 2 000×g for 10 min, the organic phase was transferred into another tube and evaporated to dryness at 40 ºC under a stream of nitrogen. The residue was reconstituted in 100 mg/L of the mobile phase and vortexed for 1 min. A 20- mg/L aliquot of the solution was injected onto the LC-MS-MS system.
To determine total daidzein (free plus conjugated daidzein), 100 mg/L β-glucuronidase enzyme solution (1084U/mL in 0.05 mol/L NH4H2PO4 buffer, pH 5.0) was added to a 50 mg/L aliquot of rat plasma. The mixture was incubated in a water bath at 37 ºC for 16 h. After enzymatic hydrolysis, 50 mg/L internal standard and 50 mg/L water were added. The mixture was treated as described above.
Those plasma samples whose concentrations were higher than the highest calibration point were diluted appropriately with blank rat plasma in order to make the concentration within the range of the standard curve before sample preparation.
The concentration of daidzein-7-O-glucuronide was calculated using the following formula:
CDG = (Ct–Cf)?430/254,
where CDG was the mass concentration of daidzein-7-O-glucuronide (conjugated daidzein), Ct was the total mass concentration of daidzein, Cf was the mass concentration of free (unconjugated) daidzein, and 254 and 430 were the molecular weights of daidzein and daidzein-7-O-glucuronide, respectively.
Study design Eighteen Wistar rats (Grade II, Certificate N
Polyethylene cannulas were implanted in the femoral vein 2 d before the experiment while the rats were anesthetized with pentobarbital (50 mg/kg, ip). The cannulas were externalized at the back of the neck and filled with heparinized saline (20 000 U/L). One group of 6 rats weighing 224±13 g were dosed orally with daidzein solution at 20 mg/kg (10 mL/kg, 2 g/L), the second group of 6 rats weighing 230±16 g were dosed orally with daidzein suspension at 20 mg/kg (10 mL/kg, 2 g/L), and the third group of 6 rats weighing 227?10 g were dosed intravenously with daidzein solution at 20 mg/kg (10 mL/kg, 2 g/L). Serial blood samples (0.25 mL) were collected at 0 h, 5 min, 10 min, 30 min, 1 h, 3 h, 5 h, 8 h, 12 h, 24 h and 48 h post dose. Plasma was separated by centrifugation at 2 000×g for 10 min and stored frozen at -20 ºC until analysis.
Data analysis Plasma concentrations were subjected to an appropriate pharmacokinetic analysis on mean data points. Values below the quantification limit were considered to be zero. The peak concentration (Cmax) and the corresponding peak times (tmax) were determined by visual inspection of the mean data. The elimination half-life (t1/2) was calculated using the non-compartmental model of the TOPFIT program on a personal computer. The area under the plasma concentration-time curve (AUC) from time zero to the last measurable plasma concentration point (t=48 h) (AUC0–48 h) was calculated using the linear trapezoidal rule. Extrapolation to time infinity (AUC0–∞) was calculated as follows:
AUC0–∞=AUC0–48 h +C48 h/ke,
where C48 h was the last measurable plasma concentration and ke was the elimination rate constant. The bioavailability (F) of free daidzein was calculated as follows:
F=AUC0–∞, po/AUC0–∞, iv,
where AUC0–∞, po and AUC0–∞, iv were the AUC values of free daidzein after oral and intravenous administration of daidzein. The bioavailability (F) of total daidzein (free plus conjugated daidzein) was calculated as follows:
F= AUC0–∞, po/AUC0–∞, iv,
where AUC0–∞, po and AUC0–∞, iv were the AUC values of total daidzein after oral and intravenous administration of daidzein.
The main pharmacokinetic parameters, including t1/2, ke, tmax, Cmax, AUC0-48 h, AUC0–∞, and F, were analyzed using the Student's t-test. A probability level of P<0.05 was defined as being statistically significant.
Results
Mass spectrometry Using the positive APCI mode, the analyte and internal standard formed predominately protonated molecules [M+H]+ in full-scan spectra. To determine daidzein using the SRM mode, full-scan and product-ion spectra of daidzein and internal standard were investigated under the present HPLC conditions. Figure 2 shows the product ion spectra of [M+H]+ ions of daidzein and genistein. Several fragment ions were observed in the product-ion spectra. The major fragment ions at m/z 199 and 153 were chosen in the SRM acquisition for daidzein and genistein, respectively.
Method validation Selectivity was assessed by comparing the chromatograms of 6 different batches of blank rat plasma with the corresponding spiked plasma. Figure 3 shows the typical chromatograms of a blank plasma sample, a blank plasma sample spiked with daidzein at the LLOQ and genistein, and a plasma sample from a Wistar rat 30 min after oral administration. No significant interference from endo-genous substances with analyte or genistein were detected. The typical retention times for daidzein and genistein were 2.7 min and 2.9 min, respectively.

Calibration standards were prepared by spiking 50 µL of the appropriate standard solutions of daidzein to 50 µL of blank rat plasma. Plasma concentrations were 0.24 µg/L, 0.50 µg/L, 1.5 µg/L, 20 µg/L, 100 µg/L, 500 µg/L and 1000 µg/L for daidzein. The linear regression of the peak area ratios versus concentrations was fitted over the concentration range of 0.24 µg/L-1000 µg/L in rat plasma. A typical equation of the calibration curve was as follows:
y=3.888?10-4+6.030?10-4 x (r=0.9981),
where y is the peak area ratio of daidzein to genistein, and x is the concentration of daidzein. The present assay method had an LLOQ of 0.24 µg/L with an accuracy of 14.3% and a precision of 12.7% (n=5), which was sufficient for monitoring daidzein plasma levels over a period of 48 h after a single oral administration.
Table 1 summarizes the intra-day and inter-day precision and accuracy for daidzein from QC samples. In this assay, the intra-day and inter-day precisions ranged from 3.4% to 7.1% and from 6.3% to 13.2% for each QC level. The accuracy ranged from -0.5% to 2.4%. The results, calculated using a one-way ANOVA, indicated that the values were within the acceptable range and that the method was accurate and precise[12].

Full table
The extraction recovery of daidzein, determined at 3 concentrations (0.50 µg/L, 50 µg/L, 800 µg/L), were 73.8%, 75.1% and 76.3% (n=6), respectively. The extraction recovery of genistein was also investigated as 64.2% (n=6).
Daidzein in the plasma was shown to be stable for at least 30 d stored at -20 ºC. The relative error (RE%) of daidzein between the initial concentrations and the concentrations of the following 3 freeze-thaw cycles ranged from -6.7% to 2.4%, which indicated the stability of daidzein during freeze-thaw. Processed samples were also found to be stable in the reconstituted solution of acetonitrile-water-formic acid (80:20:1, v:v:v) for at least 24 h at room temperature. These data are summarized in Table 2.

Full table
Pharmacokinetics The mean plasma concentration versus time curves of daidzein and daidzein-7-O-glucuronide after oral administration of 2 different dosage forms (daidzein solution and suspension) are given in Figure 4. The mean plasma concentration versus time curves of daidzein and daidzein-7-O-glucuronide after intravenous administration of daidzein solution are given in Figure 5. Table 3 summarizes the pharmacokinetic parameters of daidzein and daidzein-7-O-glucuronide after administration of 2 different dosage forms. The pharmacokinetic parameters of daidzein and daidzein-7-O-glucuronide after intravenous administration of daidzein solution are given in Table 4.



Full table

Full table
Pharmacokinetics of daidzein After oral administration of 2 different dosage forms, the absorption of daidzein after administration of daidzein solution (tmax=0.46 h) was more rapid than that of suspension (tmax=5.00 h). The peak plasma concentration after administration of daidzein solution was 601.1 µg/L, which was approximately 4 times higher than that of suspension (127.3 µg/L). The absolute bioavailability of daidzein in rats after administration of daidzein solution was 12.8%, but the absolute bioavailability of daidzein after administration of daidzein suspension was only 6.1%.
There are significant differences of daidzein parameters in the values of tmax and Cmax (P<0.05) between daidzein solution and suspension.
Pharmacokinetics of daidzein-7-O-glucuronide After oral administration of 2 different dosage forms, absorption of daidzein after administration of daidzein solution (tmax=0.40 h) was more rapid than that of suspension (tmax=3.67 h). The peak plasma concentration after administration of daidzein solution was 3000 µg/L, which was approximately 14 times higher than that of suspension (192.6 µg/L). The absolute bioavailability of total daidzein (free plus conjugated daidzein) in rats after administration of daidzein solution was 47.0%, but the absolute bioavailability of total daidzein (free plus conjugated daidzein) after administration of daidzein suspension was only 12.2%.
In general, there are significant differences between the main pharmacokinetic parameters of daidzein and daidzein-7-O-glucuronide after administration of 2 different dosage forms (P<0.05). There is better absorption following administration of daidzein solution than after administration of suspension.
Discussion
Daidzein shows poor hydrophilicity and lipophilicity due to the typical plane structure of the isoflavones. However, it can be dissolved in weak alkaline solution and form a sodium salt at the hydroxyl groups; as a result its water solubility is greatly increased to 2 g/L. Daidzein solution was found to be stable during a period of at least 24 h (data not shown).
In present study, we choose solution and suspension as the 2 representative dosage forms. Daidzein suspension has similar in vivo processes to solid preparations, while daidzein solution is a typical liquid preparation. As a compound with poor solubility, the form of administration may have a great influence on its absorption and pharmaco-kinetics.
After oral administration, daidzein is subject to glucuroni-dation at its 7-hydroxyl group, and glucuronide conjugate is its main metabolite and the form in which it mainly exists in vivo. The pharmacological effects of daidzein-7-O-glucuronide have not been reported in the literature. Daidzein can transform into daidzein-7-O-glucuronide as a substrate of glucurotransferases, and daidzein-7-O-glucuronide can transform back into daidzein by the action of a hydrolase. As a result, it is necessary to determine the concentrations of free daidzein and daidzein-7-O-glucuronide in order to study its absorption and pharmaco-kinetics.
Previous studies, which focused on the pharmacokinetics after consumption of known amounts of soy foods or limited purified isoflavones (solid preparations), found that daidzein was absorbed poorly[6?10]. In our investigations, there are significant differences in pharmacokinetic parameters of daidzein and daidzein-7-O-glucuronide between solution and suspension. After administration of daidzein solution, daidzein is absorbed well and is mostly metabolized into daidzein-7-O-glucuronide. The reason for the significant differences was the poor solubility of daidzein.
Wojcicki et al[13] reported that there were no statistically significant differences in the pharmacokinetics and bioavailability of flavonoid glycosides of Ginkgo biloba (quercetin, kaempferol and isorhamnetin) after a single oral administration of 3 formulations to healthy volunteers, which seems to contradict the results of the present study. How-ever, the 3 formulations adopted in that report were capsules, drops and tablets, which were all solid formula-tions, while in present study, solution and suspension (solid) formulations were prepared to investigate their pharma-cokinetics. In fact, there does exist significant differences in the pharmacokinetic parameters of solid and liquid formula-tions.
Pharmacokinetic parameters varied a great deal among individuals, indicating great inter-individual variability of daidzein disposition in vivo, which is in accordance with the results found in the literature[9]. There were more factors to affect the pharmacokinetic behavior of daidzein and daidzein-7-O-glucuronide after oral administration compared with using an intravenous dose, and this may be the reason that larger RSD values of AUC0−48 h were achieved after oral administration (88.2% for oral solution and 50.9% for oral suspension; 27.3% for intravenous solution). Furthermore, different distribution amounts of β-glucuronidase in vivo and strong hepatic-intestinal cycles may also account for the large differences in the amounts of daidzein and its main metabolite daidzein-7-O-glucuronide in vivo.
In conclusion, dosage forms have a great influence on the bioavailability of daidzein. Solution preparations are more bioavailable than solid preparations. As a result, the solution preparations of daidzein are recommended for development in order to improve its oral bioavailability.
References
- Pereira MA, Barnes LH, Rassman VL, Kelloff GV, Steele VE. Use of azoxymethane-induced foci of aberrant crypts in rat colon to identify potential cancer chemopreventive agents. Carcinogenesis 1994;15:1049-54.
- Anderson JJ, Anthony MS, Cline JM, Washburn SA, Garner SC. Health potential of soy isoflavones for menopausal women. Public Health Nutr 1999;2:489-504.
- Cassidy A, Bingham S, Setchell KD. Biological effects of a diet of soy protein rich in isoflavones on the menstrual cycle of premenopausal women. J Clin Nutr 1994;60:333-40.
- Thomas BF, Zeisel SH, Busby MG, Hill JM, Mitchell RA, Scheffler NM, et al. Quantitative analysis of the principle soy isoflavones genistein, daidzein and glycitein, and their primary conjugated metabolites in human plasma and urine using reversed-phase high-performance liquid chromatography with ultraviolet detection. J Chromatogr B 2001;760:191-205.
- Yasuda T, Kano Y, Saito K, Ohsawa K. Urinary and bilary metabolites of daidzin and daidzein in rats. Biol Pharm Bull 1994;17:1369-74.
- Bloedon LT, Jeffcoat AR, Lopaczynski W, Schell MJ, Black TM, Dix KJ, et al. Safety and pharmacokinetics of purified soy isoflavones: single-dose administration to postmenopausal women. Am J Clin Nutr 2002;76:1126-37.
- Busby MG, Jeffcoat AR, Bloedon LT, Koch MA, Black T, Dix KJ, et al. Clinical characteristics and pharmacokinetics of purified soy isoflavones: single-dose administration to healthy men. Am J Clin Nutr. 2002;75:126-36.
- Fischer L, Mahoney C, Jeffcoat AR, Koch MA, Thomas BF, Valentine JL, et al. Clinical characteristics and pharmacokinetics of purified soy isoflavones: multiple-dose administration to men with prostate neoplasia. Nutr Cancer 2004;48:160-70.
- Setchell KD, Faughnan MS, Avades T, Zimmer-Nechemias L, Brown NM, Wolfe BE, et al. Comparing the pharmacokinetics of daidzein and genistein with the use of 13C-labeled tracers in premenopausal women. Am J Clin Nutr 2003;77:411-9.
- Watanabe S, Yamaguchi M, Sobue T, Takahashi T, Miura T, Arai Y, et al. Pharmacokinetics of soybean isoflavones in plasma, urine and feces of men after ingestion of 60 g baked soybean powder (kinako). J Nutr 1998;128:1710-5.
- Chen XY, Qiu F, Zhong DF, Duan XT, Liu CX. Validated liquid chromatography-tandem mass spectrometric method for the quantitative determination of daidzein and its main metabolite daidzein-7-O-glucuronide in rat plasma. Pharmazie 2005;60:334-8.
- Shah VP, Midha KK, Findlay JW, Hill HM, Hulse JD, McGilveray IJ, et al. Bioanalytical method validation: A revisit with a decade of progress. Pharm Res 2000;17:1551-7.
- Wojcicki J, Gawronska-Szklarz B, Bieganowski W, Patalan M, Smulski HK, Samochowiec L, et al. Comparative pharmacokinetics and bioavailability of flavonoid glycosides of Ginkgo biloba after a single oral administration of three formulations to healthy volunteers. Mater Med Pol 1995;27:141-6.

