Comparison of drug abuse in Germany and China1
Introduction
Drug abuse has a long history in Germany and China. Drug abuse, mainly the abuse of heroin, has spread quickly since re-emerging as a national problem in China in the late 1980s. The major drug-related problem is the spread of HIV, which has caused major social and economic damage in China. China approves the methadone maintenance treatment (MMT) program, which began in 2003, and the number of clinical sites of MMT exceeded 300 by November 2006. The China Central Government adopted many strategies in the antidrug campaign in the last 10 years; however, the epidemic of drug abuse and spread of drug-related diseases like HIV/AIDS in the country are still not completely under control. With the progress of modernization, China is more open to learn from developed countries such as Germany in its struggle with drug abuse.
Germany, the largest developed European country, has faced severe heroin abuse problems since the 1970s and has had some successful experiences in controlling drug abuse, particularly in controlling the spread of HIV/AIDS. For example, the German Narcotics Act was revised in 1992 and clarified that substitution treatment for opioid dependence was legal. Since the early 1990s, substitution treatment has been the most important part of the treatment options for opioid dependence. The overall number of participants in drug-substitution treatment has risen over the past decade from about 1000 in the late 1980s to 65 000 in 2005. Although the MMT has been evaluated comprehensively in Germany with favorable outcomes, there is still a lack of availability of and accessibility to substitution treatment. In addition to opioids, the abuse of “new” types of drugs, including three, 4-methylenedioxymethamphetamine (MDMA), and ketamine has spread recently in Germany. Drug abuse has caused many problems for both abusers and the community. In response, the Germany Cabinet adopted the “Action Plan on Drugs and Addiction”; the China Central government approved a similar regulation in the antidrug campaign in 2005.
Due to the increase of drug addicts and drug-related diseases, the governments of these 2 nations have begun an antidrug campaign, including legislative measures to control drug abuse and enforce the MMT program. This review will compare the characteristics of drug abuse in Germany and China. The experiences of Germany and China have provided many beneficial methods and these experiences may be the foundation of future collaborations between Germany and China.
Situation of population and economics in Germany and China
Facts and figures Germany is one of the most important countries of Europe, both in economic power and population. Located approximately at the center of Europe, Germany has a population of 82 800 000 and area of 356 910 km2 (Figure 1). Germany is a society of immigrants. For economic, demographic, and humanitarian reasons, immigration has become an important issue for German society over the past 50 years; over 14 million people with a migrant background live in Germany today. They are either immigrants themselves or second generation immigrants. One of 5 marriages is binational and 1 of 4 children born in Germany has at least 1 foreign parent. One in 3 teenagers in West Germany has a migrant background, while in some areas, this is almost 40% and increasing. Immigration has substantially changed the constitution of Germany society; ethnic, linguistic, cultural, and religious diversity have for a long time been a living reality in Germany.
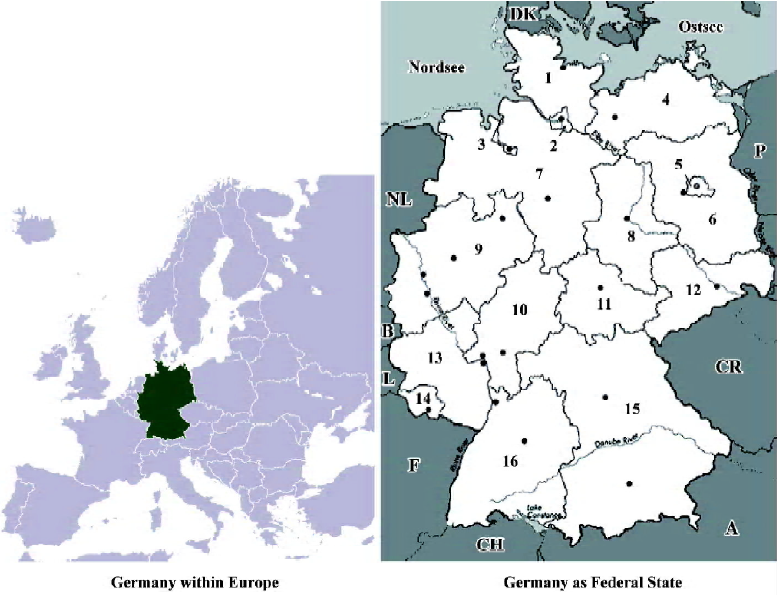
China is situated in eastern Asia on the western shore of the Pacific Ocean, with an area of 9.6 million sq km. China is the most populous country in the world with 1.25909 billion people at the end of 1999, about 22% of the world’s total population. China is a united multi-ethnic nation of 56 ethnic groups. As the majority of the population is of the Han ethnic group (accounting for 91.6% of the national total population), China’s other 55 ethnic groups are customarily referred to as the national minorities. The Constitution of China guarantees the basic rights and interests of its citizens. Adopted in 1982, China’s Constitution has been amended 4 times. The Supreme People’s Court is the highest judiciary agency in China and is responsible to the National People’s Congress and its Standing Committee.
Economic policy strategies Germany faces the challenges of globalization, and the transition to a knowledge investment in research and development amounts to 2.5% of its gross domestic product (GDP), placing it in the upper third among industrialized nations. Germany possesses an efficient society only if there is a high level of dynamism for innovation. Germany’s overall economic infrastructure for basic and applied research is among the top nations for inventions. The German economy is more profound than other countries characterized by a clear weakness in growth. Unemployment figures remain high and a noticeable decline in employment subject to social insurance contributions leads to further gaps in the social security systems, thus contributing to their considerable financial problems. More growth is therefore an essential prerequisite for tackling Germany’s current and future economic and financial problems.
With its GDP growing at an annual rate of 9%, economists predict that China’s GDP will come second after that of the USA. Such an economy market stands to offer exciting business and capital market opportunities to foreigners over the next 10 years or so. China’s annual GDP growth has averaged more than 8% in the past 25 years, and in 2005, its GDP grew by a record-breaking 9% despite the outbreak in 2003 of severe acute respiratory syndrome (SARS).
Social assistance Social assistance in Germany is intended not only to prevent poverty, but also to enable recipients to lead a dignified life. Anyone unable to do so with his or her own resources receives social assistance. There is assistance from the community for everyone who is unable to help themselves and cannot count on other support. For this reason, the regulations to enhance this self-help are particularly significant. It is fundamentally irrelevant whether beneficiaries have caused the hardship themselves. There is a legal right to almost all social assistance benefits. Anyone who is in need receives individual assistance in which his or her personal and economic conditions are accommodated. Social assistance can be provided as personal assistance, a cash benefit, or as a benefit in kind.
China’s social affairs have fallen far behind its quick economic development. About 85% of investment in sanitation flows into the urban area, while only 15% is invested in the rural area where three-quarters of the population live. Social administration in China remains at a low level due to the legacy of planned economy. The private economy needs to move into the social services, including hospitals, schools, and scientific research institutions.
Health insurance In Germany, an insured person can claim measures for the prevention and early detection of certain diseases; medical and dental treatment, with free choice among panel doctors and dentists; medicines; hospital treatment; and social therapy for insured persons who have a severe mental affliction that prevents them from accepting or taking medical treatment. State health insurance also covers the family at no extra charge. From 1 January 2004, health insurance met the cost of medical treatment for social assistance recipients who lacked statutory health insurance. Their equal status with members of the statutory health insurance schemes brought recipients of social assistance under the statutory guarantee of appropriate and affordable health-care provision.
The Chinese health-care system was originally a highly centralized one. It had great success in improving people’s health. The county-township-village 3-tier health-care system has contributed much to rural primary health care and has set an example of primary health care to developing nations. In the 1980s, this system experienced transformations along with changes of the country’s administrative system and economic policy. The long-existing health administrative problems that were aggravated in the last decade are the rural-urban differences in resource allocation and the large proportion of people without health security. With the increase of medical service prices in recent years due to the inflation of the economy, it is believed that the cost of health care will create an economic burden to low-income, fee-for-service paying individuals and will further affect the health of the population. In the process of the national economic reform, it is an important and difficult task for the health administrators to adjust the health-care system promptly and properly. Continuously carrying forward good traditions, correcting mistakes, and consistently persisting in health reforms can further raise its health care to a new, prosperous stage[1].
Drug abuse in Germany and China
Consumption and abuse of psycho-active substances After heroin had found its way onto the illegal drug market in Germany around 1970, there was a rapid increase in the number of heroin users and addicts from none to around 30 000–40 000 within only a few years. This number increased until the 1990s to 150 000–170 000 and is now slowly decreasing. During the early 1970s, “psychedelic” substances like cannabis and Lysergids (LSD) became part of a youth subculture movement, although LSD nowadays plays only a marginalized role.
With respect to illicit drugs, the use of cannabis outranks all other drugs in Germany. More than one-quarter of all young people have had experience with the drug and around 200 000, most of whom are young people, are daily users. Reports of risky consumption patterns and multiple drug use of youths and drug addicts are on the rise. The number of people seeking drug counseling centers has doubled in recent years. There is an estimated 150 000 people addicted to heroin and other opiates and about 300 000 people use cocaine regularly. In some cities, there is an increase in the consumption of crack. In the party and techno scene, the prevalence of cannabis and ecstasy consumption is almost 10 times as high as in the same age bracket outside of this “scene”. Around 500 000 people, predominantly young people, consume what is known as party or club drugs, such as ecstasy; most often mixed with other illicit drugs, such as cannabis and cocaine, but also with legal drugs such as alcohol[2].
Drug abuse in China can be traced to the late Qing Dynasty (1644–1911 AD), when British colonists forcefully brought Indian opium into China in exchange for silk, tea, and cash. Opium was then locally planted. By the founding of new China in 1949, more than 20 million Chinese people were opium addicts, representing 5% of the total population[3]. After a short nationwide antidrug campaign, drug abuse was reported to be eliminated from the mainland in the early 1950s, and for the next 3 decades, China was believed to be a drug-free nation[4].
Illicit drugs re-emerged in China in the 1980s as China adopted an open-door policy, and the re-emergence was mainly connected with global drug trafficking activities. Since the late 1990s, increasing amounts of amphetamine-type stimulants (ATS) and other chemically-related synthetic drugs, including amphetamine, methamphetamine, and ecstasy have been locally manufactured and consumed in China[5].
The number of drug users officially documented by Chinese public security departments increased from 70 000 in 1990 to 1.16 million in 2005[6], while the estimated number is currently 3.5 million. The lifetime prevalence rates of illicit drug use among residents aged 15 years or older in high prevalence Chinese cities increased from 1.1% in 1993 to 1.6% in 1996, and the 1 year prevalence rate increased from 0.9% to 1.2% during this period[7].
The main drug of choice in China is heroin. According to a report of the National Narcotic Control Commission, 87.6% of drug users abused heroin in 2002[8]. The abuse of ATS and MDMA (methylenedioxymethamphetamine or ecstasy) has become popular in city nightclubs in recent years[9].
Heroin abuse Calculations based on the figures collected from treatments, police contacts, and drug-related deaths have led to the number of problem heroin users in Germany estimated at being between 70 000 and 172 000 people. This corresponds to a rate of 1.6–3.0 people per 1000 inhabitants between the ages of 15 and 64 years[10]. Calculations based on treatment data, including clients with cocaine and amphetamine problems, produce a prevalence of 137 000–221 000 (2003: 132 00–214 000).
With heroin, intravenous use slightly decreased to 66.6% relative to the previous year (2003: 70.2%; 2002: 68.4%; and 2000; 69.5%). With cocaine, the portion of injection drug users (IDU) slightly increased to 34.3% (2003: 33.8%, 2002: 29.7%; 2001: 32.5%; and 2000: 32.8%). For the year 2004, the German addiction aid statistics recorded data based on International Classification of Diseases (ICD) 10 of a total of 38 978 people who started treatment in an outpatient psychosocial addiction aid facility because of problems with illicit drugs. More than half of the cases have been diagnosed as being opiate addicts, followed by cannabis and cocaine. For people treated for the first time, cannabis ranks first among these clients[10].
Opiate abuse in China dates back several centuries. The British supplied Indian opium to China as early as the 16th century[11], and the growth of opium use resulted in huge public health problems. By 1906, China had 13.5 million addicts consuming some 39 000 tons of opium, and an estimated 27% of its adult males were dependent on opium. This astounding level of mass addiction was probably the largest in world history[12]. By the time of the founding of the People’s Republic of China in 1949, there were over 20 million opium abusers (5% of the population) in the country and 25% of the population of the Yunnan province were opium abusers[13]. Throughout history, Chinese governments have embarked on numerous campaigns to control opium. These attempts included the well-known Opium Wars[13,14]. However, only 1 such attempt succeeded. In the early 1950s, the Chinese Government took a series of dramatic steps to combat wide-spread opium abuse, carrying out a nationwide antidrug campaign[13,15] that included the following measures: (i) a circular order was issued by the new Government in 1950 mandating governments at all levels to fight opium abuse; (ii) those involved in the cultivation, manufacture, or sale of opium were subject to severe punishments, including forced labor and execution; (iii) compulsory “treatment” was instituted (consisting largely of enforced abstinence) for opium abusers combined with psychological “rehabilitation” and vocational training programs (involving forced labor); and (iv) the cultivation, manufacture, and use of medicinal opium was closely controlled to ensure medical use[16]. During the campaign, people involved in growing opium, transporting, or trafficking illegal drugs were punished. Labor camps and executions were among the measures employed. The campaign lasted 3 years from 1950 to 1952. According to official accounts, 20 million opium addicts were detoxified and returned to healthy, useful lives[13]. Some US authors celebrated the success of the Chinese Government’s approach to the opium epidemic[17]. Official accounts, as well as some US authors, also claimed that the value system of young people had changed so that there was no new supply of addicts[17]. However, there were no rigorous epidemiological studies measuring the prevalence of opiate dependence before and after the campaign. Despite those serious limitations in our ability to rigorously evaluate how patterns of opiate use changed in the 1950s, it seems clear that the rates of dependence did decline precipitously, as the risks associated with the trade and use of opium climbed considerably. In addition, the availability of opium was curtailed dramatically by the aggressive eradication of opium planting and domestic manufacturing domestically and blocking international trafficking. China’s political and economic isolation at that time was a key factor which excluded foreign supplies of opiates.
Opiate abuse was thus rare in China prior to the establishment of closer ties with the West, beginning in 1978[11]. However, as Chinese economic development accelerated in the 1980s and China began to open its borders, opium and heroin once again entered China from the Golden Triangle region, especially through Myanmar, through the Yunnan and Guizhou provinces, to Canton (Guangzhou) and Hong Kong[18]. In the 1990s, drug-related crime grew dramatically and opiate abuse spread quickly. During the last decade, China has experienced a rapid increase in illicit drug use, predominantly heroin. From 1990 to 2006, the numbers of drug abusers officially documented in China increased more than 11-fold from 70 000 to 1 160 000[19,20].
In contrast to the information available from the 1950–1980s, which consists entirely of Government estimates, some well-designed independent epidemiological studies of more recent rates of opiate abuse are beginning to emerge. Hao et al[7,21] reported the prevalence, patterns, and trends of illicit drug use in the general population of selected high-prevalence areas (Yunnan, Sichuan, Gansu, and Guangdong Provinces) in China between 1993 and 2000. They screened more than 50 000 individuals aged 15 or above in the community and interviewed possible abusers. They found the lifetime prevalence of illicit drug use to be 1.08%, 1.60%, and 1.52% in consecutive surveys conducted in 1993, 1996, and 2000, respectively. The 1 year prevalence rates were 0.91%, 1.17%, and 1.17%, respectively. Heroin was the most common drug of abuse (51.8% in 1993, 83.4% in 1993, and 95.9% in 2000). The 2 most frequent routes of drug administration were inhalation (89.2% in 1993, 60.1% in 1996, and 93.5% in 2000) and intravenous injection (27.2% in 1993, 31.0% in 1996, and 25.7% in 2000).
Many reports have shown that the majority of addicts in China are young (30 years or younger), single (60%) males (60%–70%) with little education and without stable jobs[22–25]. Routes of administration vary depending on geographic area and year of survey. Most studies conducted after 2000 showed that intravenous injection accounted for 50%–70% and ”chasing the dragon” (zhui-long: ingestion of the drug by inhaling the vapor produced when the drug is heated to a level at which it sublimates) accounts for 25%–50% of opiate administration by users. The use of intravenous heroin is growing, with many users changing from zhui-long to the intravenous route. Finally, new drugs are now making their way into China, especially in urban areas where methamphetamine and other synthetic stimulants, as well as dissociative anesthetics, such as ketamine, are increasingly popular among young people[4,24].
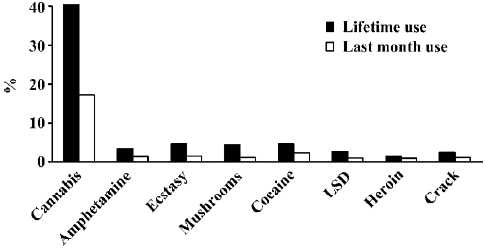
Psychostimulants, cannabis, and other new-type drugs Experience with cannabis is most common among young people in Germany, followed by mushrooms, amphetamines, and ecstasy with markedly lower prevalence; all other drugs are even less commonly found. The development of drug consumption during the lifetime and in the previous 12 months can be well compared with the data of the drug affinity study which has been collecting comparative data for the 12–25 year age group since 1979 (Figure 2). While drug experience during the lifetime increased from 16% in 1979 to 32% in 2004, current consumption in the last 2 surveys was below the level of 1997. This clearly indicates that a similar or even higher number of people have used drugs once in their lifetime, but frequency or at least the duration of consumption must have declined considering the lower prevalence figures for current consumption[10].
In the late 1990s, studies about the use of ecstasy and other so-called party drugs in Germany showed that the most common age for using ecstasy for the first time was between 16–18 years[26–31]. The motives given as “highly applicable” and “applicable” are feelings of happiness, elation, and more intense hearing and feeling. In addition, over 50% of ecstasy users report expanded consciousness, greater ease of making contact, relaxation, and overcoming personal inhibitions as being applicable to themselves[2,32,33]. About 80%–95% of people have already experienced nicotine, cannabis, and alcohol prior to using ecstasy for the first time. About 40% have experience with speed, cocaine, and LSD. Experience with psilocybin and heroin is found only very rarely[34].
In the non-organized leisure-time sector, drug prevention and especially measures relating to night life is an exception to the regular help offer in contrast to schools and working life where drug prevention activities are firmly embedded[35]. The goal of the projects and measures is to reach young people at risk (especially by involvement of peers), prevent them from starting to take addictive substances, or respectively motivate them to quit early. The activities deployed at parties range from information stalls, counseling, cultural offers, and relaxation techniques to structural measures like the sale of alcohol-free drinks at a lower price than alcoholic drinks, freely available cool drinking water, chill-out areas, cooperation with local players (eg competent authorities), as well as trained staff for medical emergencies.
It is being tried to an increasing extent to use the Internet to establish low-threshold contact with young people having a drug affinity in order to inform them, to promote critical reflection of their own consumption behavior, and to provide online support to reduce or stop their consumption or to refer them to other local help services[34,36].
In China, as the number of drug addicts increases and the drug abuse problem spreads, the consumption of traditional drugs grows alongside increasing use of new kinds of drugs. It has been reported that although opiates, especially heroin, remain the most commonly used drugs, MDMA and methamphetamine have recently become popular recreational drugs in large or medium-sized Chinese cities[37,38]. MDMA belongs to the class of ATS and is a synthetic drug that can be manufactured in 2 ways: from benzyl methyl ketone or from ephedrine extracted from the medicinal herb ephedrine[39–41]. The increasing illicit manufacture of ATS, particularly methamphetamine, in East and South-East Asia is a major concern. It has been estimated that more than 70% of all seizures of amphetamine in the world took place in East and South-East Asia, mainly in South Korea, Japan, China, and Thailand[9,42,43].
A dramatic increase in MDMA trafficking has occurred throughout the region and illegal MDMA laboratories have been discovered in mainland China, Hong Kong, Taiwan, Malaysia, and most notably, Indonesia[9]. The increased demand for ecstasy and the ready availability of precursor chemicals from China and Vietnam make South-East Asian nations increasingly vulnerable to becoming havens for large-scale MDMA manufacture[9,42]. In China, the countryside also faces a growing problem of ATS abuse[44].
HIV/AIDS and hepatitis in Germany and China
Drug users are the fourth largest risk group for HIV infections in Germany. HIV incidence is at 6% in the group of injecting drug users. Until the year 2000, the figure was at 10% and in the mid 1980s it was at 20%. Data from outpatient counseling facilities show a prevalence of 3%–4%. However, it should be noted that recent, large-scale studies allowing for a certain generalization of data are missing.
Basic data on viral hepatitis are available for the general population. According to the Federal health report, 5%–8% of the German population aged between 18 and 79 years is affected by a hepatitis B infection. A total of 0.5%–0.7% of the population carries hepatitis C antibodies[10,45]. As for the possible methods of transmission, intravenous drug use was the most commonly used method as reported by 7% of hepatitis B cases. With respect to hepatitis C, intravenous drug use at any time was most frequently reported by 37% of the cases as the most preferred route of transmission. In the 20–29 year age group for male cases, intravenous drug use was reported to be the commonly used method by 71% of cases. In summary, the antibody prevalence (infection rate) of hepatitis B among IDU in Germany is estimated to range between 40% and 60%, and for hepatitis C, the range is between 60% and 80%. While the data do not permit precise estimates, it is clear that the antibody prevalence in IDU is very high for hepatitis B and C.
MMT is the major basis for treatment of HIV/AIDS-related illnesses among drug users. The high retention rate and good compliance with treatment regimes makes treatment with antiretroviral medications feasible, whether or not it is carried out in the specialized outpatient clinics[46]. Long-term substitution programs allow observations of the antiretroviral treatment and a better response to side-effects. There are numerous potential drug interactions between antiretroviral medications and methadone and other substitute substances. Adaptations of the methadone dosage may be necessary. The analgesic properties of opioid may mask early symptoms of serious side-effects of HIV medications. A good relationship between doctor and patient is essential to deal with these problems. While in the past, IDU have usually been excluded from standard HCV therapy with interferon and ribavirin in Germany, recent results suggest a different approach[47]. Comparisons were made regarding the use of medication among drug users and non-drug users because of the following criteria: response rate, outcome of the HCV standard therapy, as well as the severity of neuropsychological side-effects[48] .
In a controlled prospective study, no differences were found in people displaying an addiction-related or psychological disorder or in a control group without such disorders with regards to psychiatric complications and response rates. However, drug users had a higher dropout rate[49]. Based on these studies and other surveys, the provisional conclusion is that HCV-infected patients who intravenously take drug may be successfully treated with standard therapies. Even in the case of light or moderately severe additional psychological disorders, HCV treatment may be carried out successfully provided on an interdisciplinary basis. The MMT is generally a prerequisite for the successful additional treatment of HIV or hepatitis in opiate-addicted individuals[48].
In Asia and the Pacific, drug abuse has led to many problems, in particular HIV/ AIDS. More than 1 million people were diagnosed with HIV in 2003, bringing the total to 7.2 million infected people in the region[50,51]. The growth of the epidemic in this area is largely due to the growing epidemic in China, in which 1 million people are living with HIV. China’s AIDS epidemic began in the early 1990s among injecting heroin users[52,53]. Injecting drug users account for more than half of China’s HIV infections. In addition, many of China’s sex workers inject drugs, and thus provide a bridge for HIV transmission to the general population[54–56]. As the commercial sex industry has exploded in China over the past 2 decades, HIV infection rates have also increased dramatically[52,55]. By the end of 2003, the number of registered HIV infections was 62 159 (including 2693 cases of AIDS from which 1047 people died). An estimated 106 990 Chinese people were HIV positive by the end of 2004. HIV infections have been reported in 31 provinces, autonomous regions, and municipalities, and the actual number of cases and spread of infection is much likely to be greater[52,53]. Drug abusers accounted for 63.7% of HIV cases. China is now one of the 6 South-East Asian countries in which there is growing ATS use, and vulnerability to HIV/AIDS appears to have increased[52,57]. It is well known that AIDS affects not only patients, but also their families, society, and the economy. China’s first law targeting the disease was passed by the Standing Committee of the National People’s Congress in 2004. Discrimination against the victims of infectious diseases has also been outlawed. Many efforts and measures have been adopted by the Central Government to help patients obtain effective treatment. As for preventing HIV spread among drug addicts, some places in China, such as Guangzhou province, are instituting needle exchange programs among drug abusers in order to break the HIV–heroin connection. Some areas are also advocating 100% condom use among sex workers.
About 170 million Chinese are infected chronically with the hepatitis B virus (HBV) and 10% suffer from chronic hepatitis. Around half a million Chinese people die from hepatitis B because of hepatocellular carcinoma and end-stage cirrhosis each year. A pilot study demonstrated that the HBsAg rate reached the adult level before the fifth year of age, and neonatal vaccination with either plasma-derived or recombinant hepatitis B vaccines provided a similar 75% protective efficacy against HBV infection. The high rate of follow up and blood test coverage of the cohorts provided data showing 75% protection at the tenth to eleventh year of age against serum HBsAg and against prolonged hepatic dysfunction. The strategy of controlling hepatitis B nationwide was based on the universal immunizations of newborns, beginning in cities and then rural areas. The large-scale vaccine source was provided by domestic plants through technology transfer, first providing plasma-derived vaccine that was replaced completely by recombinant DNA vaccine in 1997. An official survey in 1999 using a sample of 25 878 children from 31 provinces reported an average coverage rate of 70.7% using 3 doses of hepatitis B vaccination, and was found to be higher in urban areas. The Ministry of the Public Health of China has planned to integrate hepatitis B vaccination into the nationwide expanded program on immunization (EPI) program with Government-provided vaccines starting 1 January 2002[58].
MMT in Germany and China
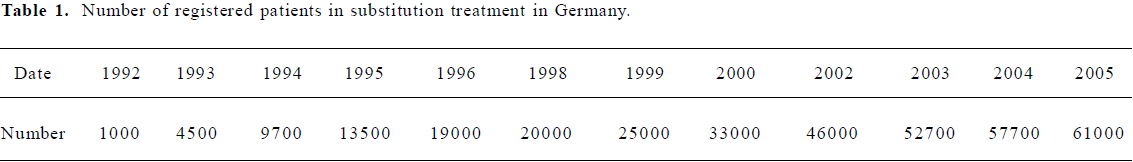
Government policy for MMT In Germany, substitution treatment has meanwhile become a central element of opioid dependence management[59–63]. Throughout the 1970s and 1980s, the drug policy of German governments remained dominated by a rigid adherence to the abstinence paradigm. The therapeutic ideal of permanent abstinence for all opiate users was considered the only valid premise for providing practical survival support and the only valid criterion for successful addiction treatment. There was an overall predominance of drug-free therapy and therapeutic community (TC) was proclaimed as the “royal road to recovery”. Until the early 1990s, methadone could only be administered to drug users when highly specific indication criteria were met (eg emergency cases, such as life-threatening conditions of withdrawal or conditions of severe pain). In general medical practice, however, German doctors were prevented from using methadone to treat heroin addicts, since MMT was considered medical malpractice. Nevertheless, there were a few general practitioners (GPs) who ignored the legal regulations and prescribed methadone to opiate addicts. The legal basis of substitution treatment was established in 2001 in the Narcotics Act and the Narcotic Drugs Prescription Ordinance. The substitution guidelines developed by the German Medical Association in 2002 are the technical basis for substitution treatment. They uphold abstinence from the substance of addiction as the prime treatment endpoint, whereby securing the individual’s survival, stabilizing their health and social situation, and enabling their professional rehabilitation and social reintegration are considered preliminary stages within a comprehensive treatment concept. Substitution treatment also fulfils preventative functions, such as prevention of infectious diseases. Substitution treatment is supposed to be accompanied by psychotherapeutic and psychosocial measures[62,64]. The Federal Institute for Drugs and Medical Devices keeps the substitution register on behalf of the Federal Laender. The tasks of the substitution register include, in particular, to prevent the multiple prescription of substitutes by several medical practitioners to 1 patient, checking compliance with the minimum requirements for the addiction therapy qualification of medical practitioners, and circulating statistical evaluations to the competent regulatory authorities and higher health authorities of the Laender. In 2002, 46 000 patients were recorded; the total number became 61 000. The number of physicians providing substitution treatment is currently around 2700. The most widely reported substitute is methadone. It is notable, however, that the proportion of buprenorphine has been rising over recent years[65,66].
Meanwhile, in accordance with the World Health Organization (WHO) “Guidelines of HIV and AIDS in Prisons”, which recommend that “prisoners on methadone maintenance prior to imprisonment should be able to continue this treatment while in prison”, substitution treatment is available in prisons in Germany. However, the implementation is the responsibility of each of the 16 Federal states (Laender) and even varies from prison to prison. Only 6 of the 16 Federal states provide substitution treatment in prisons. It is estimated that less than 700 inmates participate in substitution treatment whereas at least one-third of the 10 000 intravenous drug users in prisons on an average day should be eligible for substitution treatment. Admission criteria vary between the states and long-term maintenance treatment is often not an option. Substitution treatment is known to be an effective response in lowering the risks and harms of opioid-dependent prisoners by reducing heroin use, drug injecting and needle sharing, and prison-based drug trade. The provision should be broadened[67–70].
To what extent MMT should be included in China in the treatment strategy has been the subject of controversial discussion for a decade. Physicians involved in the management of drug addicts and investigators usually support this form of treatment, since it has clear positive effects, such as preventing HIV infection or other harm related to drug addiction. However, considerable moral objections persist over whether it is justifiable to supply drug-dependent people with an addictive substance for a prolonged period of time or for life at the tax payers’ expense. On the other hand, high recidivism rates in short-term methadone treatment and drug-free forms of treatment highlight the need to introduce maintenance treatment. Insofar, it was only consistent that the Chinese Government should have decided to carry out pilot studies in particularly affected regions (Yunnan, Guizhou, Sichuan, Zhejiang, and Guangxi). The first results show that MMT leads to a reduction in injecting drug use and criminal behaviors as well as an improvement in social behavior. Some author[71,72] advocate the combination of methadone treatment with motivating discussion techniques (motivational interviewing) and behavioral therapy elements to enhance retention rates and outcome.
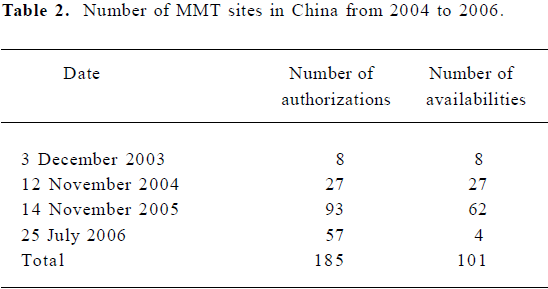
In recent years, China has seen an expansion in harm reduction-oriented programs as a strategy for addressing the drug and HIV problem. Nevertheless, there is scant experience with long-term maintenance treatment. Methadone-based withdrawal regimens have been performed in China since 1993. At first, methadone was very difficult to procure and only a few facilities (clinics) had trained staff to implement them. While treatment safety and effectiveness are also acknowledged in China, long-term treatment regimens are still being piloted. The first 8 MMT clinics were set up in early 2004, with another 26 in late 2004. In late March 2006, it was reported that 128 methadone clinics had been set up in the 3 preceding years and the number had increased to more than 300 by the end of 2006.
In the framework of the “WHO Collaborative Study on Substitution Therapy of Opioid Dependence and HIV/AIDS in developing countries in Asia and transition countries in Europe”, the Beijing Drug Withdrawal Center and the Chinese National Institute on Drug Dependence participated in the implementation and evaluation of long-term methadone maintenance treatment. In Beijing in 2005, 10 275 heroin addicts were registered as undergoing treatment (largely short-term substitution for detoxification). The average age was 32 years (men: 32.4 years, women: 30.1 years) with a marked increase over 1998 (when it was approximately 29 years). About 67.4% of heroin addicts were unemployed, 21.4% were in private business (self-employed with a low income), 2.9% were farm workers, 2.2% blue- and white-collar workers, and 1.6% were employed in the public service.
The results of the methadone treatment are convincing; both the health status and quality of life of addicts have improved significantly. The severity of dependence clearly decreased by more than half. The development of depression fell from 51% to 33%. Neither the HIV rate (3.9%) nor hepatitis C rate (46%) increased. Moreover, high-risk consumption patterns, such as injecting, were reduced signi-ficantly. However, there were no effects in terms of less risk-fraught sexual behavior. By contrast, crime rates dropped to 0 and the rate of employment increased from 25% to 31%. Retention rates were 97% after 3 months and 85% after 6 months. The average methadone dose was 39 mg at the beginning and stabilized at 49 mg per day after 6 months.
MMT is an effective method for reducing illicit opiate consumption. MMT can substantially improve the health status of those affected and enhance individuals’ quality of life. However, there are yet only 2 minor MMT programs in Beijing and they need to be expanded. Although treatment costs are 10 Yuan (about 1 Euro) per day, the financial resources needed to scale up the program are not available.
Number of MMT sites It is estimated that about 90% of substitution patients in Germany receive their medication from doctors in independent medical practices (GPs), not in clinics. However, specialized teams mostly run these practices and the clients are nearly exclusively drug addicts. In a survey from spring 1996 in a West German region, 70% of all social health insurance-approved methadone prescriptions in the area were from GPs, 20% from specialists in internal medicine, and 6% from psychiatrists. About 50% of GPs in MMT have up to 10 patients, 40% up to 40 patients, and 10% have more than 40 patients. Seven eight percent of the 61 000 patients get treatment in specialized outpatient services (with their own psychosocial staff), 20% in practices which are also treating other patient groups, but that offer special services for drug users, and (only) 4% in “normal” practices with family doctors (Table 1)[59]. Therefore, nearly 40%–60% of heroin addicts are reached by MMT.
Full table
In order to control spread of AIDS among drug takers, China plans to set up 1000 clinics that offer methadone maintenance treatment in next 5 years, and 200 000 drug takers will receive such treatment. So far, more than 10 000 people have received the treatment in China (Table 2). The working group has approved establishing the second batch of 300 clinics by June 2006. It is predicted that the number of clinics will reach 1000 by the end of 2007. There are about 840 000 HIV carriers in China in 2006 and sharing injection equipment has become the principal way for the spread of AIDS. In the MMT, drug takers will eventually reduce their dependence on heroin by taking methadone under doctors’ instructions. The treatment can also decrease the spread of AIDS caused by the sharing of injecting equipment[73].
Full table
Implication of MMT in China An important factor for the success of the MMT is support from the municipality involved. This would also include training for the local political leadership. Moreover, the dropout rate in the Chinese programs is too high (30%–40%), and unfortunately, the good results in Beijing cannot be transferred to all provinces. In order to reduce the dropout rate requires training of clinic staff and in addition, training centers should be set up in all provinces affected. Another requirement is the regular exchange of experience among the clinics. Moreover, some clinics have problems in obtaining methadone. It is necessary to introduce ethical standards for treatment and to involve nursing staff more strongly. Experience in Hong Kong specifically indicates that nurses are vital and their work is more cost-effective. In addition, there is the need for easy access to clinics and additional psychosocial interventions, such as motivational interviewing. It is assumed that a positive, basic attitude of staff towards the program critically contributes to its success. Moreover, we should bear in mind that this is a long-term program. In Hong Kong, for instance, some patients have been attending this program for as long as 20 years, which is life-maintaining for them, even though they continue to take opiates.
Experiences of methadone clinics from Yunnan (one of the most affected regions) indicate the importance of supporting self-help groups, such as Narcotics Anonymous, for sustained treatment success. The clients are given the opportunity to express their points of view. Moreover, methadone treatment in Yunnan was also integrated in drug-free programs that the methadone-maintained individuals can use. Time will tell if China can manage to implement its ambitious plans. This will result in cooperation options with other countries that have longer and positive experience with maintenance and substitution programs. This will certainly include the experience of Germany and the expert knowledge available there.
Current drug policy for harm reduction Over the past decade, Germany has moved towards harm reduction in its policies and practices regarding illicit drug use and related problems. This has been in response to the rising rates of HIV/AIDS, drug-related crime, and mortality. Germany approved the prescription of methadone[74-76] and legalized needle/syringe exchanges in the early 1990s[10]. More recently, the Federal Government legalized supervised injection sites and approved heroin trials[14,15]. The Social Democrat/Green Party Coalition Government of Chancellor Schroeder, which came to power in 1998, established new national priorities and shifted responsibility for demand and harm reduction from the Home Office to the Ministry of Health. The Government also appointed a drug commissioner and established a multidisciplinary advisory body made up of experts from the field. The Drug Commissioner’s reports address issues concerning both legal and illegal drugs and propose a greater focus on the social and health consequences of tobacco and alcohol use. The reports also emphasize that a variety of measures are needed to address legal and illegal drug problems, including increased public awareness, pilot projects, research, coordination with the Laender, and international cooperation.
Within the Federal structure of Germany, the responsibility, including financial affairs for the areas of health and prosecution, lies mainly with the Federal Laender. The Federal Government has the competence for the narcotic law, the penal law, the law on the execution of penalties, and the law on social security. On this basis, it defines a legal framework for drug policy and proposes certain standards.
In June 2003, the Federal Cabinet approved the “Action Plan Drugs and Addiction” presented by the Federal Drug Commissioner. It served as a framework plan of addiction policy for the next 5–10 years and replaced the “Plan to Combat Drugs” from 1990[10].
In China, in addition to cost and availability, other factors might also affect acceptability of methadone maintenance therapy, such as concerns about the safety and efficacy of the therapy[77]. Greater retention in treatment has been found to result in greater decreases in drug use, criminal activity, and unemployment[78]. The length of drug treatment has a positive association with better post-treatment outcomes[78]. However, limited experience with MMT in China shows a high rate of dropouts. International studies have shown that motivational enhancement therapy or motivational interviewing enhances treatment initiation, retention, and outcomes in MMT program[79], and adding behavioral intervention components into MMT programs increases abstinence and reduces HIV risk behaviors[80]. Policy-oriented operational research is needed in China to better understand how to increase the effectiveness of MMT and other harm reduction interventions in the Chinese context.
There are still persistent conflicts in the policy and legal landscape. The Central Government has given explicit support for harm reduction, as stated in the medium- and long-term strategic plan and the action plan. Some programs have been implemented successfully. However, in China, as in many other countries, public health and public security authorities frequently approach drug abuse from different perspectives, leading to conflicting approaches at local levels. The crackdown philosophy and detention of drug users in China reflect inconsistent interpretations of “harm reduction” and present a challenge to public health officials in implementing methadone substitution and needle-exchange programs[81]. Drug users may be reluctant to participate in these programs due to fear of being caught by police officers. It might be impossible to completely solve the dilemma in the near future, but this conflict is expected to gradually reduce for the following reasons. First, Chinese national policies for HIV prevention and control have become much more pragmatic in the past years. MMT and needle exchange programs were almost unimaginable several years ago, but now they are ready to be expanded across the country. We expect that the open policy trend will continue as the Chinese economy increasingly merges with international markets, and this trend will favor harm reduction programs. Furthermore, China’s Central Government may achieve an advantage in promoting public health policies if these policies are believed to be correct. Second, inter-agency coordination on the public health crisis has been enhanced at both the central and local governmental levels since the SARS outbreak in 2003, which reduced the potential conflict of public health policies. Public health workers should provide policy advocacy to public security authorities and help them change their traditional norms about illicit drug control and obtain their support for harm reduction. Third, operational research is needed to provide evidence on the benefits of harm reduction programs and convince policy enforcers of the need for the revision of unfavorable policy components.
Experiences of Germany and future collaboration between Germany and China
One important health policy aim is to do the utmost to prevent or at least considerably reduce risky and damaging consumption patterns as well as dependence on addictive substances in our society. Addiction prevention therefore occupies a prominent place in policy efforts. However, it is also an objective to be able to recognize risky consumption patterns at an early stage and reduce them, ensure the survival of those affected, and treat cases of dependence with all of the possibilities available according to the current level of scientific knowledge: from abstinence to medically-supported therapy. Addiction is a disease that requires treatment.
In Germany, addicts have a legal right to assistance. The bodies responsible for providing social security benefits (the health insurance funds, pension insurance funds, institutions responsible for social assistance, and the municipalities) are obliged to finance such assistance. Together with the service providers and self-help groups, they have succeeded over the past decades in making available a differentiated range of addiction and drug assistance offers that provide addicts in need of assistance with a broad spectrum of different services. Over the past 30 years in Germany, a high quality and differentiated treatment system has been developed in the area of addict assistance. This system comprises outreach and low-threshold forms of assistance, outpatient counseling and treatment offers, qualified withdrawal treatment, inpatient detoxification treatment with a subsequent adaptation phase and follow up, and post-inpatient care within the framework of integration (eg outpatient rehabilitation, special care housing, occupational rehabilitation projects, follow-up care, and self-help groups)[28,82,83]. These offers are supplemented by a medication-assisted outpatient treatment system especially for opiate addicts. Cooperation between the non-institution doctors and the addict-support system is to be promoted at the interface with acute medicine. The treatment aims are realistic and pragmatic and include the following aims:
1. To assist the patient to remain healthy until (with the appropriate care and support) they can achieve a life free of drugs.
2. To reduce the use of illicit and non-prescribed drugs by individuals.
3. To deal with the problems related to drug misuse.
4. To reduce the dangers associated with drug misuse, particularly the risk of death by overdose and HIV, hepatitis infections from injecting, and sharing injecting paraphernalia.
5. To reduce the duration of episodes of drug misuse.
6. To reduce the chances of future relapse to drug misuse.
7. To reduce the need for criminal activities in order to finance the drug misuse.
8. To improve overall personal, social and family functioning.
In Germany, a history of substitution treatment spanning 20 years has meanwhile accumulated a wealth of experience in the following areas:
· The development of health care services research
· The development of guidelines and the implementation of quality assurance measures
· The practical implementation of substitution treatment with the concomitant effects and treatment elements, such as drug history taking, dosage setting, course of other psychoactive substances (alcohol, benzodiazepines, cocaine), management of “difficult patient populations”, and integration of the social environment
· The development of a program for psychosocial therapies adjuvant to substitution treatment and in the framework of the pilot project of “heroin-based treatment”, also with standardized manuals
· Allocation research to find the “right” therapy form at the “right” point in time[84]
· The pilot project “heroin-based treatment” through experience with clients who do not benefit from methadone treatment
· Through expertise in the treatment of specific comorbidities, such as HIV/AIDS and hepatitis and psychiatric comorbidity
· The (Europe-wide) use of substitution treatment in prisons
· The promotion and involvement of self-help groups that are highly relevant
· The production, licensing, distribution, and control of substitution agents, including the setting up of a substitution register
· The framework of cooperation with the European Monitoring Center of Drugs and Drug Addiction in Lisbon, in the development of Europe-wide standards for substitution treatment.
China will definitely benefit from the successful experiences of Germany and other developed countries in controlling drug abuse and drug-related diseases.
References
- Liu XZ, Wang JL. An introduction to China’s health care system. J Public Health Policy 1991;12:104-16.
- Rakete G, Flüsmeier U. Ecstasy-Eine explorative Studie zum Konsum und Mißbrauch von Ecstasy. Wiener Zeitschrift für Suchtforschung, 1995.
- Fang YX, Wang YB, Shi J, Liu ZM, Lu L. Recent trends in drug abuse in China. Acta Pharmacol Sin 2006;27:140-4.
- Zhao C, Liu Z, Zhao D, Liu Y, Liang J, Tang Y, Liu Z, Zheng J. Drug abuse in China. Ann N Y Acad Sci 2004;1025:439-45.
- Qian HZ, Schumacher JE, Chen HT, Ruan YH. Injection drug use and HIV/AIDS in China: Review of current situation, prevention and policy implications. Harm Reduct J 2006;3:4.
- Chu TX, Levy JA. Injection drug use and HIV/AIDS transmission in China. Cell Res 2005;15:865-9.
- Hao W, Xiao S, Liu T, Young D, Chen S, Zhang D. The second National Epidemiological Survey on illicit drug use at six high-prevalence areas in China: prevalence rates and use patterns. Addiction 2002;97:1305-15.
- Annual report on drug control in China. Beijing, China National Narcotics Control Commission (CNNCC), 2002.
- Kulsudjarit K. Drug problem in southeast and southwest Asia. Ann N Y Acad Sci 2004;1025:446-57.
- Simon R, David SM, Farke W. Germany. New Developments, Trends and In-Depth Information on Selected Topics. 2005.
- McCoy CB, Lai S, Metsch LR, Wang X, Li C, Yang M, et al. No pain no gain: establishing the Kunming, China, drug rehabilitation center. J Drug Issues 1997;27:73-85.
- McCoy AW. The Politics of Heroin: CIA Complicity in the Global Drug Trade: Afghanistan, Southeast Asia, Central America, Colombia. Chicago, Lawrence Hill Books; 2003.
- Bai YT. The anti-opium campaign movement in the early 1950s. CPC History 2001;10:38.
- Baumler A. Modern China and Opium: a Reader. Ann Arbor, University of Michigan Press; 2001.
- McCoy CB, McCoy HV, Lai S, Yu Z, Wang X, Meng J. Reawa-kening the dragon changing patterns of opiate use in Asia, with particular emphasis on China’s Yunnan province. Subst Use Misuse 2001;36:49-69.
- Jiang ZN: Heroin addiction and contemporary treatments. Beijing: Science Press; 1995.
- Lowinger P. The solution to narcotic addiction in the People’s Republic of China. Am J Drug Alcohol Abuse 1977;4:165-78.
- Naik TN, Sarkar S, Singh HL, Bhunia SC, Singh YI, Singh PK, et al. Intravenous drug users — a new high-risk group for HIV infection in India. Aids 1991;5:117-8.
- Drug use and HIV vulnerability: Policy research study in Asia. Bangkok UNAIDS Asia Pacific Inventory Team, 2000.
- Shi J, Liu YL, Fang YX, Xu GZ, Zhai HF, Lu L. Traditional Chinese medicine in treatment of opiate addiction. Acta Phar-macol Sin 2006;27:1303-8.
- Hao W, Su Z, Xiao S, Fan C, Chen H, Liu T, Young D. Longitudinal surveys of prevalence rates and use patterns of illicit drugs at selected high-prevalence areas in China from 1993 to 2000. Addiction 2004;99:1176-80.
- Zhou Y, Li XL. Demographic characteristics and illegal drug use patterns among attendees of drug cessation programs in China. Subst Use Misuse 1999;34:907.
- Liu ZM, Lu XX, Mu Y, Lian Z, Zhou WH. Epidemiological features of drug abusers in China. Chin J Drug Abuse Prevent Treat 2002;8:27-30.
- Xue LY, Wang ZC, Du YJ, Fei H. Retrospective investigation of the epidemiology and characteristics of drug abuse in Shanghai. Chin J Drug Depend 2002;11:47.
- Lou JL, Shi JH, Yang HH, Li F, Zheng PK, et al. A survey of substance abuse among 2207 drug users in Yunnan. Chin J Drug Abuse Prevent Treat 2003;9:5.
- Krollpfeiffer K. Auf der Suche nach ecstatischer Erfahrung. Berlin, On the search for ecstatic experience, 1995.
- Gouzoulis-Mayfrank EHL, Kovar KA. Die Entaktogene: Ecstasy” (MDMA), Eve” (MDE) und andere ring-substituierte Methamphetaminderivate. Eine neue Stoffklasse unter den illegalen Designer-Drogen? Nervenarzt 1996;67:369.
- Wilkinson DA, Leigh GM, Cordingley J, Martin GW, Lei H. Dimensions of multiple drug use and a typology of drug users. J Addict 1987;82:15.
- Lyttle T, Montagne M. Drugs, music and ideology: a social-pharmacological interpretation of the ‘acid-house-movement’. Int J Addict 1992;27:1159.
- Griffiths PVL. The use of amphetamines, ecstasy and LSD in the European Community: a review of data on consumption patterns and current epidemiological literature. In: the EMCDDA by the National Addiction Centre (NAC). London, 1997.
- Henderson S. Women, sexuality and ecstasy use - the final report. Lifeline publication. 1993.
- Saunders N. Ecstasy. Ricco Bilgen, Zurich, 1994.
- Tossmann HP. Ecstasy-konsummuster, konsumkontexte und komplikationen. Ergebnisse der Ecstasy-Infoline. Suchtmed 1997;2:9.
- Tossmann HP, Heckmann WT. Drogenkonsum Jugendlicher in der Techno-Party-Szene. 1997.
- Lewis R, Sherval J. Demand reduction activities related to “new synthetic drugs”: MDMA (ecstasy), other amphetamines and LSD in European Member States., in Report prepared for the EMCDDA by the Centre for HIV/AIDS and Drug Studies (CHADS). Edinburgh, 1997.
- Tossmann HP, Heckmann WT. Drogenprävention für die Techno-Party-Szene. 1997.
- Center Nioddandas: Report of drug surveillance. Beijing, National Institute on Drug Dependence, 2003.
- Center Nioddandas: Report of drug surveillance. Beijing, National Institute on Drug Dependence, 2004.
- Hanson GR, Rau KS, Fleckenstein AE. The methamphetamine experience: a NIDA partnership. Neuropharmacology 2004;47 Suppl 1:92-100.
- Morton J. Ecstasy: pharmacology and neurotoxicity. Curr Opin Pharmacol 2005;5:79-86.
- Parrott AC. MDMA (3,4-Methylenedioxymethamphetamine) or ecstasy: the neuropsychobiological implications of taking it at dances and raves. Neuropsychobiology 2004;50:329-35.
- Beyrer C, Razak MH, Lisam K, Chen J, Lui W, Yu XF. Overland heroin trafficking routes and HIV-1 spread in south and south-east Asia. Aids 2000;14:75-83.
- Chung H, Park M, Hahn E, Choi H, Choi H, Lim M. Recent trends of drug abuse and drug-associated deaths in Korea. Ann N Y Acad Sci 2004;1025:458-64.
- National Anti-drug Committee, in Anti-drug forum, 2004.
- Backmund MR, Reimer J, Meyer K, Gerlach T, Zachoval R. Hepatitis C virus infection and injection drug users. Prevention, risk factors and treatment. Clin Infect Dis 2005;40 Suppl S:S330.
- Gölz J, Rockstroh J. Compliance in der HIV-Therapie. 2001.
- Gölz J, Klausen G, Schleehauf D. Therapie der chronischen Hepatitis C bei HIV/HCV-koinfizierten Drogenabhängigen. Suchtthera-pie 2006;7:2.
- Schäfer M, Heinz A, Backmund M. Treatment of chronic hepatitis C in patients with addiction: time to change the rules. Addiction 2004;99:9.
- Mauss S, Berger F, Goelz J, Jacob B, Schmutz G. A prospective controlled study of interferon-based therapy of chronic hepatitis C in patients on methadone maintenance. Hepatology 2004;40:120-4.
- Annual report of China-UK HIV/AIDS Prevention and Care Project. Beijing, China-UK Workshop on HIV/AIDS in China, 2004.
- Kaufman J, Jing J. China and AIDS: the time to act is now. Science 2002.296.
- Yang H, Li X, Stanton B, Liu H, Liu H, Wang N, et al. Heterosexual transmission of HIV in China: a systematic review of behavioral studies in the past two decades. Sex Transm Dis 2005;32:270-80.
- Zeng Y. HIV infection and AIDS in China. Arch AIDS Res 1992;6:1-5.
- Kerr C. Sexual transmission propels China’s HIV epidemic. Lancet Infect Dis 2005;5:474.
- Lau JT, Feng T, Lin X, Wang Q, Tsui HY. Needle sharing and sex-related risk behaviours among drug users in Shenzhen, a city in Guangdong, southern China. AIDS Care 2005;17:166-81.
- Ruan Y, Qin G, Liu S, Qian H, Zhang L, Zhou F, et al. HIV incidence and factors contributed to retention in a 12-month follow-up study of injection drug users in Sichuan Province, China. J Acquir Immune Defic Syndr 2005;39:459-63.
- Aceijas C, Stimson GV, Hickman M, Rhodes T. Global overview of injecting drug use and HIV infection among injecting drug users. Aids 2004;18:2295-303.
- Sun Z, Ming L, Zhu X, Lu J. Prevention and control of hepatitis B in China. J Med Virol 2002;67:447-50.
- Gerlach R, Caplehorn JRM. Attitudes and beliefs of doctors prescribing methadone to addicts in the Westfalen-Lippe region of Germany. Drug Alcohol Rev 1999;18:163.
- Degkwitz PC, Krausz M. Five years of methaone prescription in Germany, in AIDS and drug addiction in the European Commuity. Proceedings of a Seminar on AIDS and drug addiction in twelve European Comunities Member States, EMCDDA, 1993.
- Verthein U, Raschke P, Kalke J. ‘Methadone Therapy in Hamburg’. Eur Addict Res 1995;1:7.
- Michels II, Stoever H, Gerlach R. Substitution treatment for opioid dependent in Germany. Chin J Drug Depen 2006.
- Verthein U, Kalke J, Raschke P. ‘Substitution treatment with methadone in Germany: politics, programmes and results’. Int J Drug Policy 1998;9:8.
- Scherbaum N, Kluwig J, Specka M, Krause D, Merget B, Finkenbeiner T, et al. Group psychotherpy for opiate addicts in methadone maintenance treatment. A controlled trial. Eur Ad Res 2005;11:9.
- Brack JBK. Erfahrungen mit dem Einsatz von Buprenorphin in der qualifizierten stationaeren Entzugsbehandlung Opiatab-haengiger. Suchtmed 2004;6:241-8.
- Krausz M, Verthein U, Degkwitz P, Haasen C, Raschke P. Maintenance treatment of opiate addicts in Germany with medications containing codeine - results of a follow-up study’. Addiction 1998;93:1161.
- Stöver H. Drug substitution treatment and needle exchange programs in German and European prisons. J Drug Issues 2002;2:23.
- Stöver H. An overview study: Assistance to drug users in European Union Prisons. Lisbon, European Monitoring Centre for Drugs Drug Addict 2001.
- Stöver H, Hennebel L, Casselmann J. Substitution treatment in European prisons, in a study of policies and practices of substitution treatment in prisons in 18 European countries. London/Oldenburg, 2004.
- Stöver H, Casselmann J, Hennebel L. Substitution treatment in European prisons: A study of policies and practices in 18 European countries. Int J Prisoner Health 2006;2:10.
- Scherbaum N, Kluwig J, Specka M, Krause D, Merget B, Finkbeiner T, Gastpar M. Group psychotherapy for opiate addicts in methadone maintenance treatment — a controlled trial. Eur Addict Res 2005;11:163-71.
- Sigmon SC, Stitzer ML. Use of a low-cost incentive intervention to improve counseling attendance among methadone-maintained patients. J Subst Abuse Treat 2005;29:253-8.
- 1000 clinics offering methadone maintenance treatment to be opened, in People’s Daily Online, 2004.
- Newman RG. ‘Another Wall That Crumbled - Methadone Maintenance Treatment in Germany’. Am J Drug Alcohol Abuse 1995;21:27-35.
- Gerlach R. Drug substitution treatment in Germany: a critical overview of its history, legislation and current practice. J Drug Issues 2002;2:503-22.
- Newman RG. Is there a Role for Methadone in Germany? AIDS Public Policy J 1988;3:23-9.
- Rosenberg H, Melville J, McLean PC. Acceptability and availability of pharmacological interventions for substance misuse by British NHS treatment services. Addiction 2002;97:59-65.
- Simpson DD. The relation of time spent in drug abuse treatment to posttreatment outcome. Am J Psychiatry 1979;136:1449-53.
- Carroll KM, Ball SA, Nich C, Martino S, Frankforter TL, Farentinos C, et al. Motivational interviewing to improve treatment engagement and outcome in individuals seeking treatment for substance abuse: a multisite effectiveness study. Drug Alcohol Depend 2006;81:301-12.
- Schroeder JR, Epstein DH, Umbricht A, Preston KL. Changes in HIV risk behaviors among patients receiving combined pharmacological and behavioral interventions for heroin and cocaine dependence. Addict Behav 2006;31:868-79.
- Thompson D. The “People’s War” against drug and HIV/AIDS, 2005.
- Poehlke T, Flenker I, Schlüter HJ, Busch H. Suchtmedizinische Versorgung. Berlin, Provision of Addiction Medicine, 2000.
- Heather N. Treating addictive behaviors: process of change. New York: Plenum Press; 1998.
- Bühringer G. Allocating treatment options to patients profils: clinical art or science? Addiction 2006;101:646-52.
