Effective use of corticosteroids in treatment of plastic bronchitis with hemoptysis in Chinese adults
Introduction
Plastic bronchitis is a rare disorder characterized by the formation of extensive endobronchial casts[1]. A diagnosis is usually made when casts are expectorated or removed by bronchoscopy[2]. Many cases of plastic bronchitis in children have been published[3]. The processes associated with bronchial cast formation include asthma[4], allergy[5], infection[6], bronchiectasis[1], cystic fibrosis[6], and acute chest syndrome of sickle cell disease[7], and as a complication after many different congenital cardiac defects, such as the Fontan procedure[8,9].
One published study[10] showed the classification of casts based on their composition. Type 1 or inflammatory casts consist predominantly of fibrin with dense eosinophilic, lymphocyte or neutrophilic inflammatory infiltration, and are associated with underlying inflammatory diseases of the lung. Type 2 or acellular casts are composed primarily of mucin with no acute inflammatory infiltration and sometimes a few mononuclear cells. The latter casts are found more commonly in children. However Seear et al[10] did not address whether this classification aids in the treatment of these patients, apart from indicating that acellular casts carry a poorer prognosis than inflammatory casts. Because plastic bronchitis is a rare disorder associated with variable disease states, specific therapeutic options are based primarily on anecdotal experience, such as acetylcysteine[10], low-dose oral azithro-mycin[11,12], urokinase[13], extracorporeal membrane oxygenation (ECMO)[2], nebulised recombinant human Dnase[14], corticosteroids[10,15] and tissue plasminogen activator (t-PA)[16]. At present, therapy for bronchial casts remains limited[17].
Corticosteroids have recently been employed preferentially in plastic bronchitis, but this has only been reported in case reports[10,15,18], not in clinically controlled trials. In the present study, we provide a special case series of thirty-two plastic bronchitis patients with hemoptysis[18,19] in Chinese adults admitted to West China Hospital between 1996 April and 2005 June, in order to explore the clinical features and the role of corticosteroids in treatment.
Materials and methods
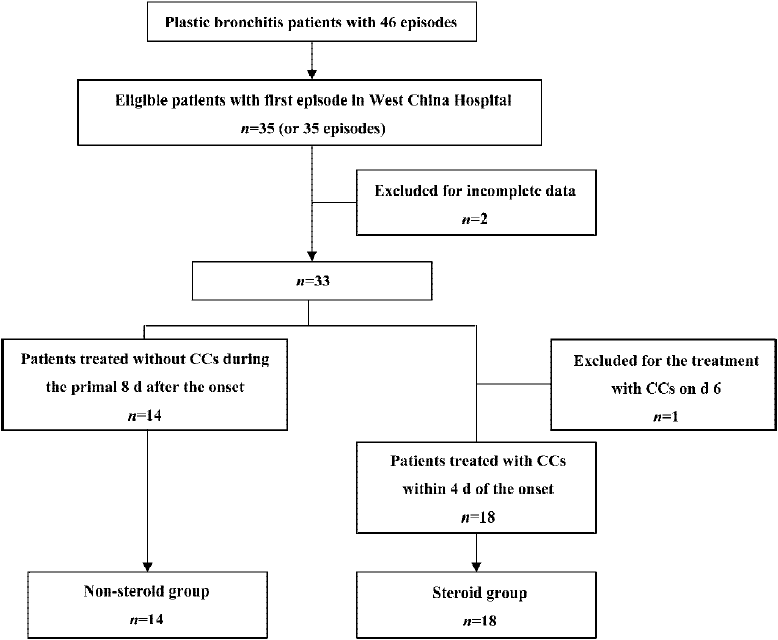
Patients and ethics From April 1996 to June 2005, West China Hospital’s databases were searched for patients who were treated for plastic bronchitis, and a retrospective review was performed of the patients’ medical records. Forty six episodes were searched but the diagnosis of plastic bronchitis with hemoptysis was made in only thirty-five patients. Two out of 35 were excluded because of incomplete data. The remaining 33 patients were divided into a steroid group and a non-steroid group. The patients in the steroid group (n=18) were treated with corticosteroids within 4 d of the onset of plastic bronchitis with hemoptysis, and only one patient who was treated with corticosteroids on d 6 was excluded. Those in the non-steroid group (n=14) were not treated with corticosteroids during the 8 d after onset (Figure 1). Furthermore, none of the patients with plastic bronchitis in either the steroid group or the non-steroid group had received any inhaled, injected, or oral corticosteroids or any immune inhibitors in the previous four weeks.
The Medical Ethics Committee of West China Hospital at Sichuan University approved this study in accordance with the recent principles of the Declaration of Helsinki[20]. The efficacy of corticosteroids in plastic bronchitis is not confirmed and this is a retrospective case-control study.
Standard interventions Patients with plastic bronchitis were immediately admitted to the medical care unit. The eight major goals in therapy were addressed uniformly in both groups: (1) monitoring temperature, pulse, respiration, blood pressure and the arterial oxygen saturation of the hemoglobin using pulse oximetry (SPO2) (Oxisensor, Nellcor, Hayward, CA, USA); (2) hemostatic agents; (3) the elimination of any identifiable underlying problem; (4) bronchodilators; (5) improved clearance of tracheobronchial secretions; (6) infection control; (7) greater rest and/or sedation; (8) mechanical ventilation for respiratory failure.
In the steroid group, patients were treated with hydrocortisone, prednisone, or methylprednisolone. A fibreoptic bronchoscopy (FOB) was performed within 3 days after hemoptysis desisted in both groups, and a biopsy was done if necessary.
Clinical variables The volume of hemoptysis and bronchitis casts of all patients who coughed up were recorded in detail. The volume of hemoptysis was calculated in a measuring cup with a scale and later blood expectoration was placed in a basin with normal saline for over 4 h, and normal saline was replaced every hour. After a few hours, bronchial casts distinctly appeared, and were delivered to the department of pathology for microscopic evaluation and the analysis of cellular composition. The bronchial casts were fixed in 10% formalin, dehydrated, mounted in paraffin, sectioned, and stained with hematoxylin and eosin (HE). Four hundred cells of a HE-stained slide preparation were counted for determination of the cellular composition.
White blood cell counts, red blood cell counts, neutrophil, eosinophil, and platelet, hemoglobin, prothrombin time (PT), activated partial thromboplastin time (APTT) in blood were determined as soon as patients arrived at our hospital. Mycobacterium and fungal stains (including pulmonary aspergillus) and cultures of the cast, purified protein derivative (PPD) skin testing, and erythrocyte sedimentation rate (ESR) were measured in the lab. Chest radiograph and computed tomographies (CT) or high resolution computed tomogram (HRCT) were also performed to identify the underlying problem after hemoptysis stopped.
Statistical analysis All continuous values were expressed as mean±SEM, and compared using the Mann Whitney U-test. Categorical data were compared using the Chi-squared test or Fisher’s exact test. Statistical analysis was performed using SPSS software for windows (Version 11.5, SPSS Inc. Chicago, IL, USA). A double sided P-value of less than 0.05 was considered to be statistically significant.
Results
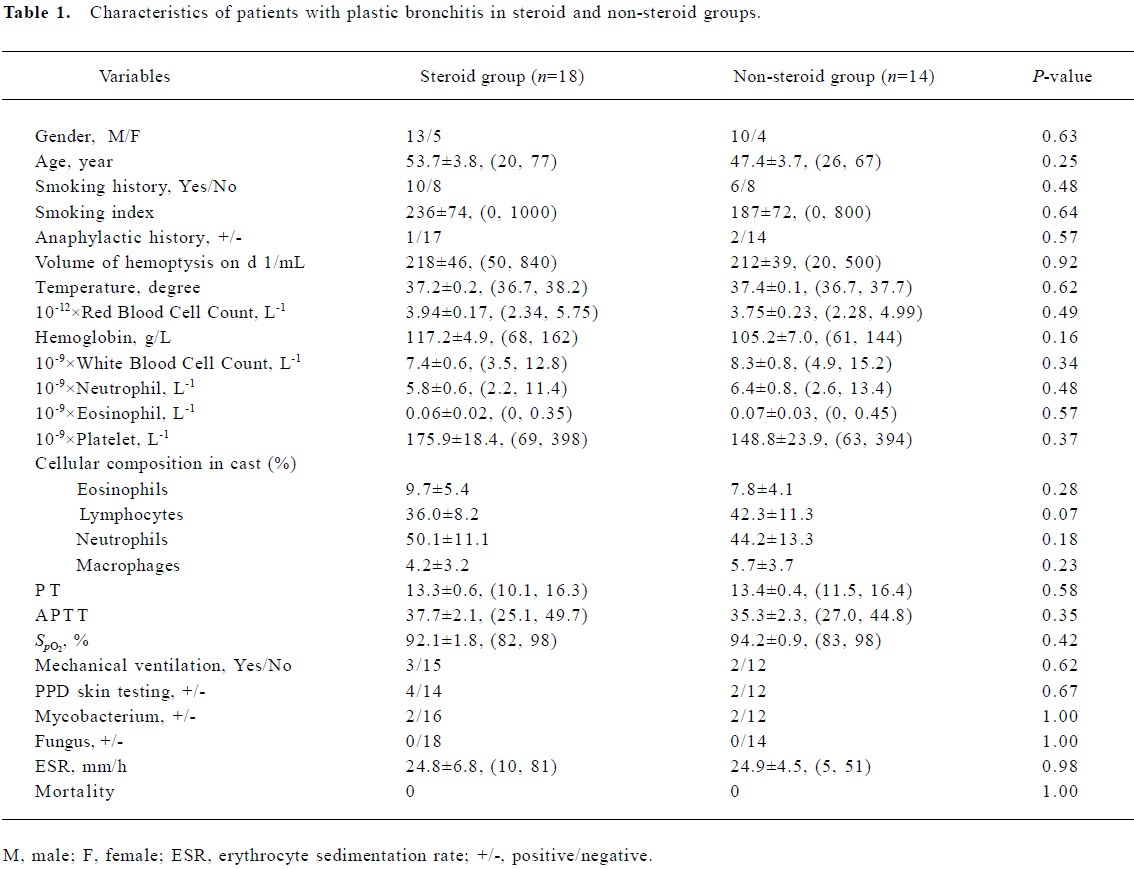
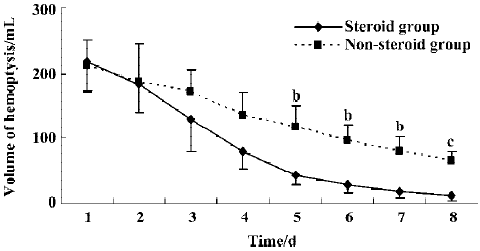
Patient characteristics There were thirteen men and five women aged 20–77 years (mean 53.7 years) in the steroid group, and ten males and four females aged 26–67 years (mean 47.4 years) in the non-steroid group. The demographic data and identifiable underlying problems of those patients are listed in Tables 1 and 2, respectively. Clinical variables, such white blood cell count, neutrophil, eosinophil, platelet, hemoglobin, SpO2, PPD skin testing, ESR, mycobacterium and fungal stains and cultures of the casts, are listed in Table 1. Fungal stains and cultures of the cast, especially aspergillus, were negative in both groups. The homogeneity test between the two groups at baseline indicated that the two groups were comparable in all aspects (all P>0.05).
Full table
Full table
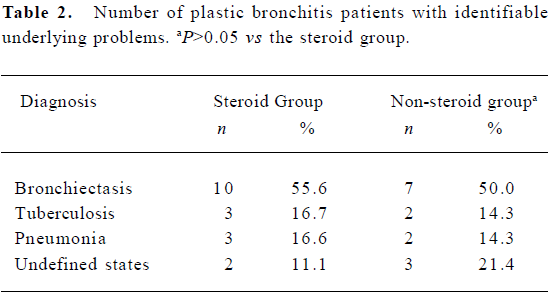
Volume of hemoptysis and bronchial casts The volume of hemoptysis was recorded in detail from when plastic bronchitis took place. On d 2, the volume of hemoptysis in both the steroid group and the non-steroid group began to decrease, but the decrease was much slower in the non-steroid group from d 2. After the 8 d treatment, the volume of hemoptysis was much more decreased in the steroid group compared with that in the non-steroid group (43±15 mL vs 117±33 mL on d 5, 29±12 mL vs 97±23 mL on d 6, 18 ±10 mL vs 80±20 mL on d 7, and 13±8 mL vs 66±14 mL on d 8, P=0.033, P=0.016, P=0.01, and P=0.002, respectively) (Figure 2).
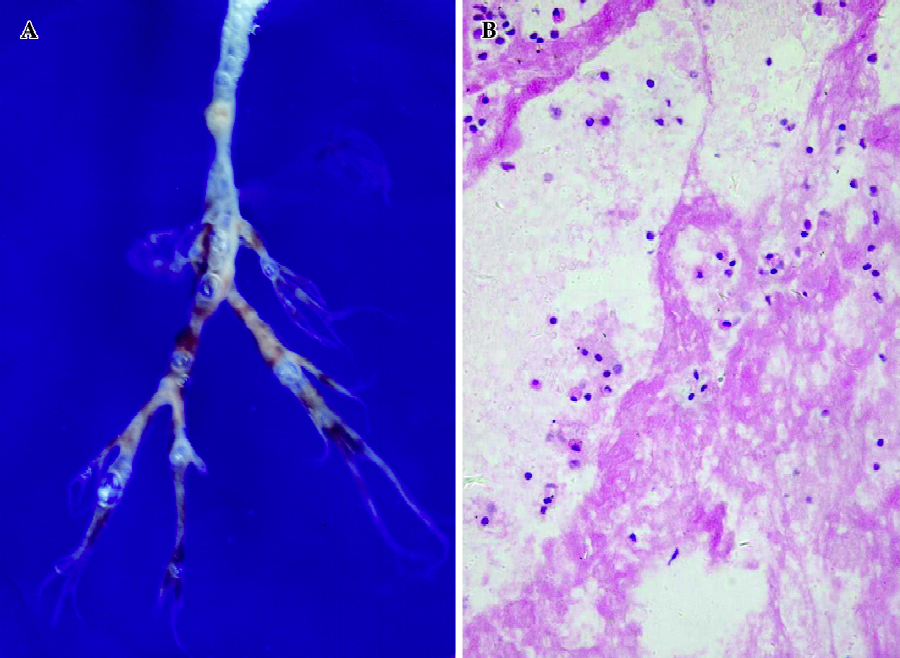
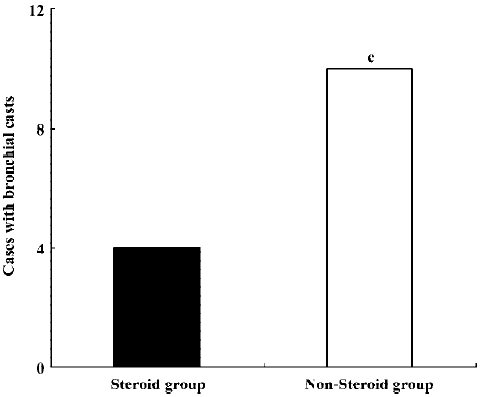
After blood was expectorated, it was placed into normal saline solution and bronchial casts eventually appeared in all cases. Bronchial casts were always with concomitant hemoptysis. The bronchial casts observed had varying consistencies and were usually soft, hollow, often ramified and white or yellowish (Figure 3A). Microscopic evaluation of the bronchial cast from every patient found that the cast consists of fibrin with eosinophils, neutrophils, lymphocytes, and macrophages (Figure 3B). There was no statistically significant difference in cellular composition of bronchial casts between the two groups (Table 1). Until d 10, FOB had been performed in eighteen patients in whom hemoptysis had desisted, but no bronchial casts were found in bronchi except for bloodstain. The cases with any bronchial casts made significant reductions in the steroid group in comparison to those in the non-steroid group (4 of 18 vs 10 of 14, P=0.005, odds ratio=7.75, 95% CI=[1.76, 43.60]) (Figure 4).
Efficacy and safety of corticosteroids Hydrocortisone, prednisone, or methylprednisolone was used in the steroid group, but corticosteroids were administered in only three patients on d 1, possibly because the diagnosis of plastic bronchitis was not made in other patients at that time. In light of the different anti-inflammation effects, all doses of hydrocortisone, prednisone or methylprednisolone were used daily in the steroid group and were calculated as the dose of dexamethasone. On d 3, the initial dose of corticosteroids had reached its peak (8.3 milligrams) and was then decreased to 7.0 milligrams as dexamethasone was maintained. At the same time, the resultant volume of hemoptysis was approximately consistent with the administration of the corticosteroid dose. Three out of 18 in the steroid group and two out of 14 in the non-steroid group received invasive mechanical ventilation for respiratory failure (P=0.62), but no deaths were found in both groups (Table 1). During the 8 d of treatment with corticosteroids, no gastrointestinal hemorrhage or other adverse events related with corticosteroids occurred in the steroid group.
Follow-up Since d 9, some patients in the non-steroid group were treated with corticosteroids because of their limited efficacy. Fifteen days later, hemoptysis stopped and no bronchial casts were found in all patients except one with bronchiectasis in the steroid group and two with undefined states in the non-steroid group. These three patients were later prematurely discharged. The dose of corticosteroids was lowered one-half every 7 d if used over 5 d.
Discussion
Plastic bronchitis is a clinical entity characterized by the expectoration of casts, which could cause obstruction of the tracheobronchial tree and respiratory distress[19]. The casts are of variable size and take the shape of the bronchi in which they form. This condition can occur at any age[10], but the majority of published reports regarding plastic bronchitis are in pediatric patients, except for a few adult patients[3,21]. In this study, 84.4% of patients had identifiable underlying problems such as bronchiectasis (53.2%), tuberculosis (15.6%) and pneumonia (15.6%), but the etiology of cast formation in a few patients (15.6%) could not be defined[22].
Plastic bronchitis with hemoptysis has been reported much more in China perhaps because of underlying problems as a developing country. The present report is different from many published reports in that we could not see the casts directly. Blood expectoration was placed into a container with normal saline for over 4 h, and normal saline was replaced every hour. Several hours later, bronchial casts distinctly appeared. Hemoptysis of large volumes (eg mean 216 mL on d 1) in those patients occurred while bronchial casts were expectorated. Usually, it was too difficult for this kind of hemoptysis to be cured with common hemostatics. Furthermore, most patients with plastic bronchitis in our study could cough out bronchial casts formed in their tracheobronchus without the help of bronchoscopic removal[7], perhaps because of the fact that they are all of the adult population and possess good pulmonary functions.
Until now, no specific therapy for bronchial casts has been shown to be effective. Different therapies have been applied in various case reports, depending on the nature of the cast or identifiable underlying disease. Since 1997, bronchial casts were separated into two well-defined types: type 1 (inflammatory) and type 2 (acellular)[10]. However, its importance in the treatment of plastic bronchitis was not presented in recent studies. In our study, microscopic examination of these casts in all patients revealed fibrinous exudates mixed with mucin, exfoliated epithelial cells, and inflammatory cells, which were consistent with type 1 casts. Although plastic bronchitis is an uncommon disease, bronchial casts with hemoptysis could result in life-threatening airway obstruction and asphyxiation[23]. In recent studies, corticosteroids have been employed preferentially in plastic bronchitis[2,15], but without any controlled study results the efficacy of this therapy remains to be established. According to our clinical experience we put forward the hypothesis that corticosteroids were effective and safe in the treatment of plastic bronchitis with hemoptysis. In this retrospective study, the results showed that on d 2 the volume of hemoptysis in the steroid group began to decrease sharply, but in the non-steroid group the decrease was much slower. On d 5, 6, 7, and 8, the volume of hemoptysis was significantly decreased in the steroid group compared to the non-steroid group (all P<0.05). Furthermore, the cases with bronchial casts decreased evidently in the steroid group compared with the non-steroid group (OR=7.75, 95% CI=[1.76, 43.60]) until d 10. Although the volume of hemoptysis and plastic casts could be improved by corticoids, no statistical difference was found in some endpoints such as mechanical ventilation and mortality between two groups in this study.
Multiple factors are likely to interplay in the pathogenesis of bronchial casts. These include airway inflammation caused by acute respiratory tract infections as documented in our cases. This was different between our study and Western countries. Bronchiectasis and tuberculosis are common diseases in the developing world, especially in China[24,25]. Some studies have reported that the addition of corticosteroids is effectively used in the treatment of bronchiectasis and tuberculosis[26,27]. In this study, corticosteroids have been shown to be effective on the basis of common supportive therapy, but its mechanism of hemostasia or inhibiting casts formation was unclear. As mentioned above, all bronchial casts of the patients in the two groups were inflammatory. After corticosteroids were administered, hemoptysis with bronchial casts in patients of the steroid group was reduced markedly. Thus, we speculate that hemoptysis may be related to bronchial inflammation as it was not cured with common hemostatics except for corticosteroids, which could reduce inflammatory cytokine expression[28]. But the detailed correlation between hemoptysis and inflammation remains to be determined. Although plastic bronchitis, especially with type 1 casts, is described as usually a self-limited illness[29], our study suggested that corticosteroids might at least shorten the course of this disease. Unfortunately it is to be determined whether corticosteroids could decrease the risk of mechanical ventilation in plastic bronchitis patients with hemoptysis.
Because this is a retrospective case-control study with a small sample size, the differences in outcome between the steroid and non-steroid groups may be exaggerated (type 2 error). In evidence-based medicine (EBM), Dave Sackett generated “levels of evidence” for ranking the validity of evidence about the value of preventive manoeuvres, and then tied them as “grades of recommendations” to the advice[30]. Moreover, the dictates of EBM suggest that when the ideal study is not available, one falls back on the strongest evidence that one can access[31]. Therefore, although the present study had some limitations, it would be the best evidence thus far for the treatment of plastic bronchitis with hemoptysis.
Conclusion
In the present study, we proved that routine doses of corticosteroids as an anti-inflammatory drug would be effective and safe for plastic bronchitis in a clinically controlled study in China. Clinicians should intervene early with corticosteroids if bronchial casts are found in patients with large volumes of hemoptysis. Although improvement after the administration of corticosteroids was observed in this study, a multi-centre, prospective, clinically controlled trial is warranted.
Acknowledgements
We thank Xiao-dong CHEN, a medical student, for assistance with recording data, Mrs Xiao-ling WU and Mrs Lan YUAN of the medical care unit for major contributions in the daily care of these patients, and Prof Guan-jian LIU at Chinese Evidence-based Medicine and Clinical Epidemiology Centre and Prof Michael SEEAR at British Columbia’s Children’s Hospital in Canada for helpful suggestions. We also thank Jon P COLIAS at San Francisco State University for assistance with editing this manuscript.
References
- Bowen A, Oudjhane K, Odagiri K, Liston SL, Cumming WA, Oh KS. Plastic bronchitis: large, branching, mucoid bronchial casts in children. Am J Roentgenol 1985;144:371-5.
- Brogan TV, Finn LS, Pyskaty DJ Jr, Redding GJ, Ricker D, Inglis A, et al. Plastic bronchitis in children: a case series and review of the medical literature. Pediatr Pulmonol 2002;34:482-7.
- Studer SM, Terry PB. Images in clinical medicine: bronchial cast. N Engl J Med 2002;346:981.
- Liston SL, Proto D, Siegel LG. Plastic bronchitis. Laryngoscope 1986;96:1347-51.
- Kao NL, Richmond GW. Cough productive of casts. Ann Allergy Asthma Immunol 1996;76:231-3.
- Fairshter RD, Riley CA, Hewlett RI. Large bronchial casts. Arch Intern Med 1979;139:522-5.
- Moser C, Nussbaum E, Cooper DM. Plastic bronchitis and the role of bronchoscopy in the acute chest syndrome of sickle cell disease. Chest 2001;120:608-13.
- Ishman S, Book DT, Conley SF, Kerschner JE. Plastic bronchitis: an unusual bronchoscopic challenge associated with congenital heart disease repair. Int J Pediatr Otorhinolaryngol 2003;67:543-8.
- Tzifa A, Robards M, Simpson JM. Plastic bronchitis: a serious complication of the Fontan operation. Int J Cardiol 2005;101:513-4.
- Seear M, Hui H, Magee F, Bohn D, Cutz E. Bronchial casts in children: a proposed classification based on nine cases and review of the literature. Am J Respir Crit Care Med 1997;155:364-70.
- Schultz KD, Oermann CM. Treatment of cast bronchitis with low-dose oral azithromycin. Pediatr Pulmonol 2003;35:139-43.
- Shinkai M, Rubin BK. Macrolides and airway inflammation in children. Paediatr Respir Rev 2005;6:227-35.
- Quasney MW, Orman K, Thompson J, Ring JC, Salim M, Schoumacher RA, et al. Plastic bronchitis occurring late after the Fontan procedure: treatment with aerosolized urokinase. Crit Care Med 2000;28:2107-11.
- Manna SS, Shaw J, Tibby SM, Durward A. Treatment of plastic bronchitis in acute chest syndrome of sickle cell disease with intratracheal rhDNase. Arch Dis Child 2003;88:626-7.
- Onoue Y, Adachi Y, Ichida F, Miyawaki T. Effective use of corticosteroid in a child with life-threatening plastic bronchitis after Fontan operation. Pediatr Int 2003;45:107-9.
- Costello JM, Steinhorn D, McColley S, Gerber ME, Kumar SP. Treatment of plastic bronchitis in a Fontan patient with tissue plasminogen activator: a case report and review of the literature. Pediatrics 2002;109:e67.
- Madsen P, Shah SA, Rubin BK. Plastic bronchitis: new insights and a classification scheme. Paediatr Respir Rev 2005;6:292-300.
- Yuan YM, Wang YJ. Plastic bronchitis with hemoptysis: a case report. West China Med J 1998;13:404. Chinese..
- Werkhaven J, Holinger LD. Bronchial casts in children. Ann Otol Rhinol Laryngol 1987;96 1pt1:86-92.
- World Medical Association. Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA 2000;284:3043-5.
- Jett JR, Tazelaar HD, Keim LW, Ingrassia TS 3rd. Plastic bronchitis: an old disease revisited. Mayo Clin Proc 1991;66:305-11.
- Muller W, von der Hardt H, Rieger CH. Idiopathic and symptomatic plastic bronchitis in childhood: a report of three cases and review of the literature. Respiration 1987;52:214-20.
- Zhang TH, Hou SY. A death case with plastic bronchitis. J Clin Pulmonary Med 2005;10:118.
- Tsang KW, Tipoe GL. Bronchiectasis: not an orphan disease in the East. Int J Tuberc Lung Dis 2004;8:691-702.
- Tocque K, Bellis MA, Tam CM, Chan SL, Syed Q, Remmington T, et al. Long-term trends in tuberculosis: comparison of age-cohort data between HongKong and England and Wales. Am J Respir Crit Care Med 1998;158:484-8.
- Tsang KW, Tan KC, Ho PL, Ooi GC, Ho JC, Mak J, et al. Inhaled fluticasone in bronchiectasis: a 12 month study. Thorax 2005;60:239-43.
- Smego RA, Ahmed N. A systematic review of the adjunctive use of systematic corticosteroids for pulmonary tuberculosis. Int J Tuberc Lung Dis 2003;7:208-13.
- Cole PJ. Inflammation: a two edged-sword – the model of bron-chiectasis. Eur J Respir Dis Suppl 1986;147:6-15.
- Park JY, Elshami AA, Kang DS, Jung TH. Plastic bronchitis. Eur Respir J 1996;9:612-4.
- Sackett DL. Rules of evidence and clinical recommendations on the use of antithrombotic agents. Chest 1986;89 suppl:2S-3S.
- Guyatt G. Evidence-based medicine: past, present and future. Chin J Evidence-based Med 2004;4:3-7.